Completed Research
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) is present in 6-12% of men and is the most frequent urological diagnosis for men younger than 50 years old. CP/CPPS significantly reduces quality of life, even below that of other prevalent chronic conditions. CP/CPPS has varied pathophysiology. One identified mechanism for CP/CPPS is involuntary localized neuromuscular activity. Physical therapy has emerged as one primary treatment modality for CP/CPPS, but up to 41% of patients report little to no improvement or a worsening of symptoms after a course of physical therapy treatment.
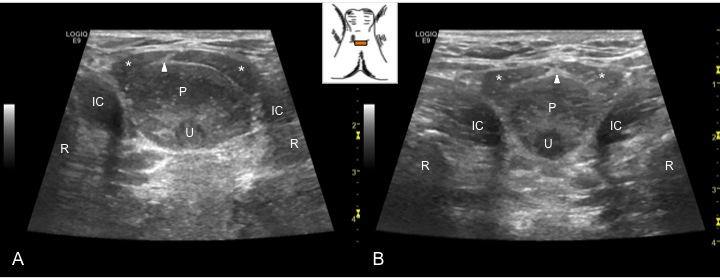
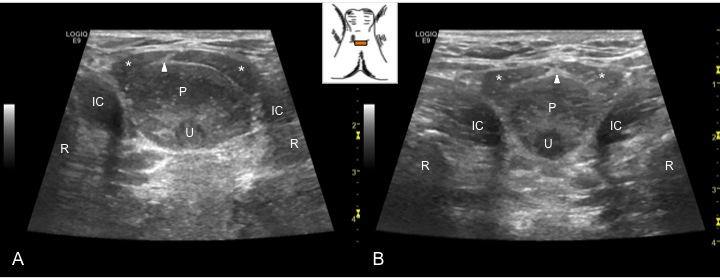
Transperineal sonographic image of the male pelvic floor in two participants, depicting the muscles (ischiocavernosus, IC; bulbospongiousus, asterisk) surrounding the urethera (u) and bulb of the penis (p), and differences in the directionality of the central tendon (arrowhead)
Our team used sonography to evaluate the physical mechanisms underlying CP/CPPS. We developed and validated a scanning protocol to evaluate the muscles of the male pelvic floor using a transperineal approach. This protocol can be used to evaluate difference among individuals with and without CP/CPPS, as well as identify variations within patients with CP/CPPS. The approach may also be useful for targeting treatments to areas of hyper-contraction (e.g., trigger points) or as a biofeedback tool to train patients in both relaxation techniques and proper exercises for these muscles.
Funding
Integrating electromyography and sonographic imaging for evidence-based PT for CPPS
Southern California Clinical and Translational Science Initiative (SC-CTSI)
Clinical Pilot Award (Co-PIs: Kutch & Roll)
Total Funding: $30,000
Funding Period: 7/1/2012 – 6/30/2013
Publications
Roll, S. C., Rana, M., Sigward, S., Yani, M., Kirages, D., & Kutch, J. (2015). Cadaveric validation and in-vivo measurement reliability of a novel linear-array transperineal sonographic evaluation of male pelvic floor structures [Electronic poster presented at the 2015 AIUM Annual Convention and Preconvention Program Hosting WFUMB Congress]. Ultrasound in Medicine and Biology, 41(4, suppl.), S103. https://doi.org/10.1016/j.ultrasmedbio.2014.12.426 Show abstract
Objectives. Rigorous reliability and validity data for emerging male pelvic floor imaging protocols has not been reported. This study validated and examined reliability of a novel linear-array, transperineal sonographic approach for evaluating superficial male pelvic floor structures.
Methods. The superficial pelvic muscles (bulbospongiosus (BS), ischiocavernosus (IC), bony landmarks, and the bulb of the penis were identified via dissection of two embalmed male cadavers. Relative depth and orientation of these structures were compared to sonograms obtained from two male participants, resulting in standardization of the imaging protocol and providing face validity for image analysis. Transverse images were then obtained from 20 male participants (GE Logiq E9, 11-Linear) at two time points. Three raters measured cross-sectional area (CSA) and linear thickness of the bulb of the penis, urethra, BS and IC muscles in three seperate trials for each of 38 images (2 participants lost to follow-up). Two-way, mixed effects intra-class correlation coefficients (ICC) were calculated within repeated trials by rater (intra-rater) and across raters (inter-rater). Minimum acceptable reliability for this study was set at 0.60.
Results. Measures of the bulb of the penis had excellent reliability (ICC > 0.90), CSA of all muscles had good reliability (ICC [0.70-0.92]), and thickness of the BS near its central tendon had good reliability (ICC > 0.80). For rater identified thickest region of the muscles and all urethra measures, reliability was poor-to-fair (ICC [0.50-0.85]) and varied widely, with most lower bounds of confidence intervals falling below the acceptability threshold (<0.60). Intra-rater reliability was similar across the three raters who had varied sonography experience and pelvic knoweldge.
Conclusions. The superficial structures of the male pelvic floor can validly identified and CSAs can be reliably measured using this sonographic approach. This approach can be used to advance knoweldge and practice for patients with pelvic disorders through the investigation of morphologic differences from healthy controls and the evaluation of clinical intervention effects.
Roll, S. C., Rana, M., Sigward, S. M., Yani, M. S., Kirages, D. J., & Kutch, J. J. (2015). Reliability of superficial male pelvic floor structural measurements using linear-array transperineal sonography. Ultrasound in Medicine & Biology, 41(2), 610-617. https://doi.org/10.1016/j.ultrasmedbio.2014.09.008 Show abstract
This study evaluated reliability of measures for superficial structures of the male pelvic floor (PF) obtained via transperineal sonography. Two embalmed cadavers were dissected to identify positioning of muscles on and around the bulb of the penis and to confirm the PF protocol. Cross-sectional area (CSA) and linear thickness of the bulb of the penis, urethra, bulbospongiosus (BS) muscles, and ischiocavernosus (IC) muscles were measured on 38 transverse images from 20 male patients by three raters with varied study knowledge and sonographic experience. Intra- and inter-rater reliability were calculated with two-way, mixed effects intra-class correlation coefficients. Measures of the bulb of the penis had the best reliability. CSA of all muscles and sagittal thickness of the BS near the central tendon had good reliability. Reliability varied for rater-identified thickest muscle region and measures of the urethra. Our study suggests that structures of the male PF can be reliably evaluated using a transperineal sonographic approach.
Roll, S. C., & Kutch, J. J. (2013). Transperineal sonography evaluation of muscles and vascularity in the male pelvic floor. Journal of Diagnostic Medical Sonography, 29(1), 3-10. https://doi.org/10.1177/8756479312472394 Show abstract
Idiopathic chronic male pelvic pain is difficult to diagnose and treat. Currently, diagnosis relies on subjective symptoms; objective measures of neuromuscular mechanisms have not been investigated. Sonographic imaging has been used to investigate these neuromuscular mechanisms in the female pelvic floor, but neither research nor books describe sonography evaluation of the male pelvic floor. The purpose of this study was to develop and evaluate a perineal sonographic technique for the examination of the male pelvic floor muscles. Anatomic landmarks were identified with images collected from two subjects, one with intermittent reports of pelvic pain and one with no history of pain in the pelvic region. A description of the equipment settings, the examination protocol, and the resulting comparative image analysis is included. A validated protocol such as this may be useful in documenting differences in the soft tissue structures between asymptomatic individuals and patients with chronic pelvic pain to aid in diagnosis and treatment. This is the first known study to report sonographic findings of the individual muscles in the male pelvic floor, and additional research is needed to validate the techniques that have been deemed feasible.
Complete Presentation List
Roll, S. C., Rana, M., Sigward, S., Yani, M., Kirages, D., & Kutch J. (2015). Cadaveric validation and in-vivo measurement reliability of a novel linear-array transperineal sonographic evaluation of male pelvic floor structures. Research poster presented at the 15th World Congress of Ultrasound in Medicine and Biology, Orlando, FL.
Roll, S. C., & Kutch, J. J. (2014). Reliability of transperineal sonographic evaluation of male pelvic floor structures. Poster presented at USC Ostrow School of Dentistry Research Day, Los Angeles, CA.
Roll, S. C., & Kutch, J. J. (2013). Transperineal sonographic evaluation of the male pelvic floor. Poster presented at USC Ostrow School of Dentistry Research Day, Los Angeles, CA.
Rana, M., Roll, S. C., & Kutch, J. J. (2013). Identifying muscle hyperactivity in chronic pain. Poster presented at USC Ostrow School of Dentistry Research Day, Los Angeles, CA.


Social