Research Buzz
To Be More Precise
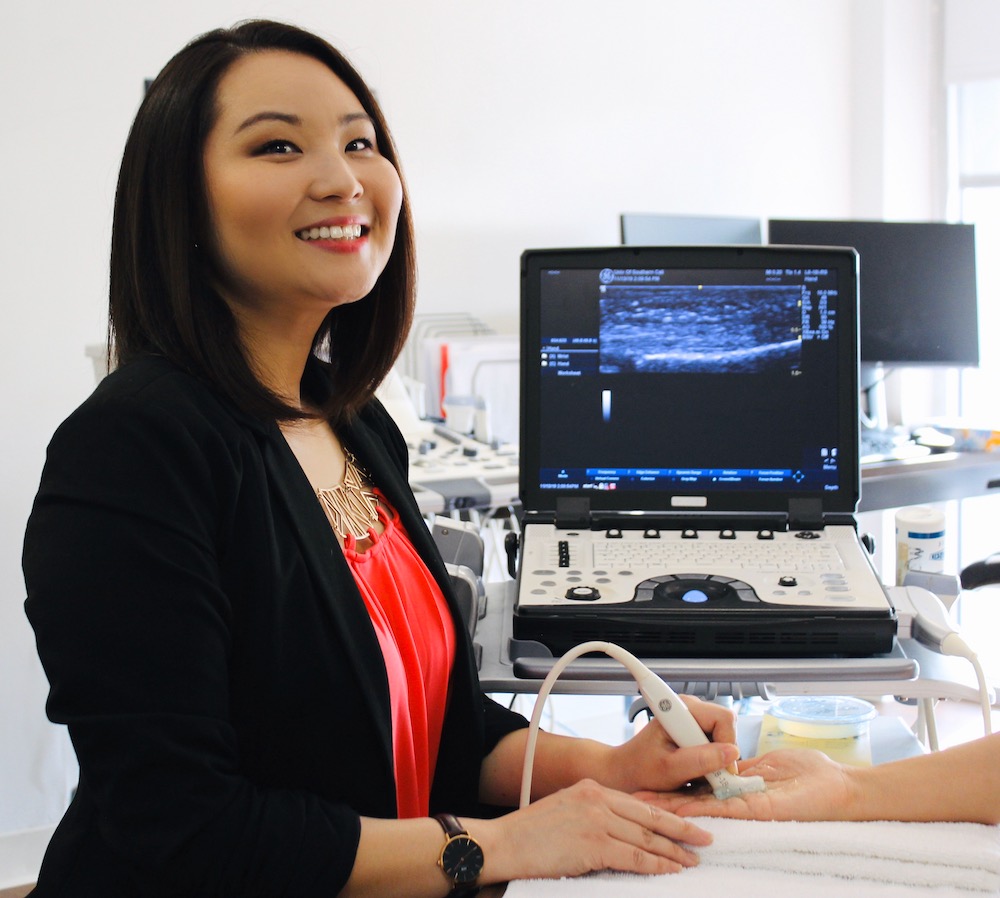
How sonographic imaging can advance rehabilitation of surgically repaired hand tendons.
By Sandy Takata MA ’15, OTD ’16, PhD ’21
Occupational Science PhD Student and Awardee, NIH F31 Predoctoral Individual National Research Service Award
Acute traumatic tendon injuries of the hand occur in more than 100,000 people in the United States every year. Repairing a tendon laceration is expensive and requires surgery, with an estimated cost of over $70,000. When successfully healed, the ends of the repaired tendons are joined together in a way that allows free movement and adequate strength to complete hand-related activities. Healing can take roughly 10-12 weeks.
The timing to initiate wrist and hand motion after surgery is critical to recovery. Doing movements too early, especially during functional activities, risks rupturing the tendon repair; however, delaying motion for too long risks the development of scar adhesions that impede hand mobility and often leads to permanently limited function. Although we are aware that there are many surgical, rehabilitation and personal factors that can affect a successful tendon repair, the evidence is unclear as to when we should initiate movement for optimal functional recovery.
Given this current issue in hand therapy, my research examines a new way of evaluating when it is appropriate to initiate movement that we hope will be more efficient, safer and appropriately individualized, especially when compared to current standardized care. Specifically, I believe musculoskeletal sonography can help solve this problem. Sonography is an inexpensive, non-invasive and pain-free imaging tool that provides real-time pictures of anatomical structures beneath the skin. Clinicians can use sonography to detect healthy and problematic changes in healing tendons. In addition, researchers have identified biomarkers that correlate with immediate and long-term outcomes following tendon repairs through sonographic assessment. Important biomarkers for tendon recovery include measures of tendon thickness, edema, hypervascularization and tendon gliding.
Thanks to the NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases, I was fortunate enough to become the first ever USC Chan PhD student to receive a F31 Predoctoral Individual National Research Service Award. According to the NIH, the purpose of this competitive award is “to enable promising predoctoral students with potential to develop into productive, independent research scientists, to obtain mentored research training while conducting dissertation research.” In addition to this fellowship award, which provides mentored training, I have received funding from the Society of Diagnostic Medical Sonography and the American Hand Therapy Foundation to support data collection for my dissertation.
The focus of my dissertation research is to establish a protocol for capturing images of the healing tendon, measuring key sonographic biomarkers and relating those biomarkers to functional recovery. Using these data, we can provide robust information to the clinical and scientific community regarding successful tendon healing over time. By relating this healing process to functional recovery, we can identify indicators of successful or problematic recovery that can inform clinical decision-making. Using musculoskeletal sonography in this way can help ensure that people with tendon injuries are receiving client-centered care that is tailored to their healing process. This research will serve as an initial step towards better understanding the ideal time to initiate active motion for each individual.
As an occupational therapist who specializes in hand therapy, I am excited to leverage this training and research predoctoral fellowship award to help develop a translational model for implementing sonography into clinical rehabilitation. The opportunities provided by this award will allow me to develop proficiencies in musculoskeletal sonography, the processes of tendon healing as well as quantitative research methods and data analysis techniques.
Beyond the scope of my dissertation, I see potential uses of sonography in hand rehabilitation for treating individuals with many other upper extremity diagnoses as well. Clinicians can use sonography to observe dynamic movement of anatomical structures and evaluate how these structures interact with each other during functional activities. Even more exciting, sonography can be used to further support individualized care by measuring tissue response to interventions across time. Moreover, imaging can also aid in educating individuals about their injuries, promoting adherence to clinician recommendations or be used as a direct intervention tool, such as with real-time biofeedback.
Developing expertise in these areas and carrying out my proposed research will enable me to address some of the current problem areas in hand therapy, and will be fundamental to my becoming a leader in musculoskeletal rehabilitation research. Most importantly, I see this fellowship as a catalyst for improving our clinical approaches to musculoskeletal rehabilitation and, ultimately, the outcomes of the people whom we serve.
⋯