Student Blog
Daniel

Hola, Yo Soy un Terapeuta Ocupacional (Hello, I Am an OT) ⟩
May 11, 2021, by Daniel
Diversity First-Gen What are OS/OT?
“Hola, yo soy un terapeuta ocupacional . . .” (Hello, I am an occupational therapist). This is part of my weekly introduction with Spanish-speaking clients. It is also a reminder of the reason I pursued this profession, as well as the sacrifices my family and I have made over the last three years. Walking into a room or simply calling a new client and starting a conversation in Spanish puts a smile on my face. Every time I speak to one of my clients, I picture my mom and dad. It feels incredible to be able to advocate for people who come from a similar background as mine.
During my time at USC, I have shared many personal things with you all. I understand the privilege of being able to write and freely express myself on this platform. Not everyone gets this opportunity, so I wanted to show that my experience as an undocumented student is as valid as anyone’s. That it is okay for those reading to feel proud of their language, culture, and history. That you belong in this program and profession.
Today I write to you just a couple of days away from walking the stage for my doctoral program. It feels really strange to say that; I think it’s the impostor syndrome that lingers. My family and friends still need to remind me that this is a huge accomplishment and to take a moment to celebrate. But those who know me pretty well know that I think this is just another step in what’s to come. First-generation, undocumented students are capable of so much, and for me, it’s time to capitalize on that. This is the end of one journey but the beginning of a new one.
This grad school journey has not been easy at all. Some semesters I wasn’t even sure I would be back given the financial limitations and ongoing immigration rhetoric surrounding DACA. The people around me made it possible to pursue this dream. There are so many who helped me along the way, and I want to acknowledge them as best as possible.
Mi familia, gracias por todo, I love you so much. My parents are the most courageous people I know. Growing up, they always told my sister and me to study hard because we would end up like them if we didn’t. But as I grow older, all I want to do is be like them. Thank you to my sister and my girlfriend for always being there for me. The sleepless nights studying and finishing assignments was all for them.

The CSUN Dream Center, I am forever grateful for your mentorship and for giving me the confidence to even apply to USC. You made me believe that I could accomplish my goals despite my undocumented status.

Thank you to the Chan Division, Norman Topping Family, Latino Alumni Association, and Immigranted for supporting me when I had no idea how I would pay for OT school. You all made this moment possible.

Thank you to the LRCC Research Lab and the Student Ambassadors team; it has been an honor to work with two outstanding teams. During the pandemic, these two teams faced many obstacles, adjusted, and we got things done! I have worked with two of the best bosses in the Chan Division, Kim Kho and Dr. Beth Pyatak.

Thank you to all my classmates who challenged me and helped me grow. A special thank you to Katie Bui and Marilyn Rodriguez, two people who always had my back since day one.

Lastly, a special thank you to Dr. Celso Delgado (el profe). You became a mentor to me throughout this entire OT experience. You reminded me that I belong in these spaces, that a Latinx kid from Van Nuys could make it.

So, this it! I have never been good at saying goodbye; I tend to simply move on and take on whatever is next. I want to take a final moment to honor my ancestors and the generational sacrifices that it took for me to get to this point. This right here is what our parents believed in as they decided to migrate. But I don’t want to be remembered as “the successful immigrant” because all immigrants, undocumented people, etc. deserve the same level of respect and acknowledgment as the “educated ones.” I had different opportunities and circumstances. Para toda mi gente Latinx y indocumentada, este logro es por todos ustedes, nosotros seguiremos luchando y echandole ganas. Although I don’t know for certain what my future looks like in this country, I do know one thing, that I will always continue to Fight On! No one can ever take away what I’ve accomplished these past years and my soon-to-be title, Dr. Daniel Padilla Vega.

⋯

A Week in the Life: OTD Residency Edition ⟩
April 30, 2021, by Daniel
Classes Fieldwork Life Hacks Videos
As I prepare to go into the last semester of my OTD Residency, I wanted to share with you all what a typical week looks like for me. Completing my residency at the LAC+USC Primary Care Adult West Clinic has been one of the most rewarding experiences I’ve had as a student, and now licensed occupational therapist.
I hope you find this vlog helpful and enjoy it!!!
If you have any questions, feel free to reach out to me at .(JavaScript must be enabled to view this email address) or .(JavaScript must be enabled to view this email address).
⋯

Mixed Status Families ⟩
March 29, 2021, by Daniel
Admissions Classes Diversity Fieldwork Life Hacks
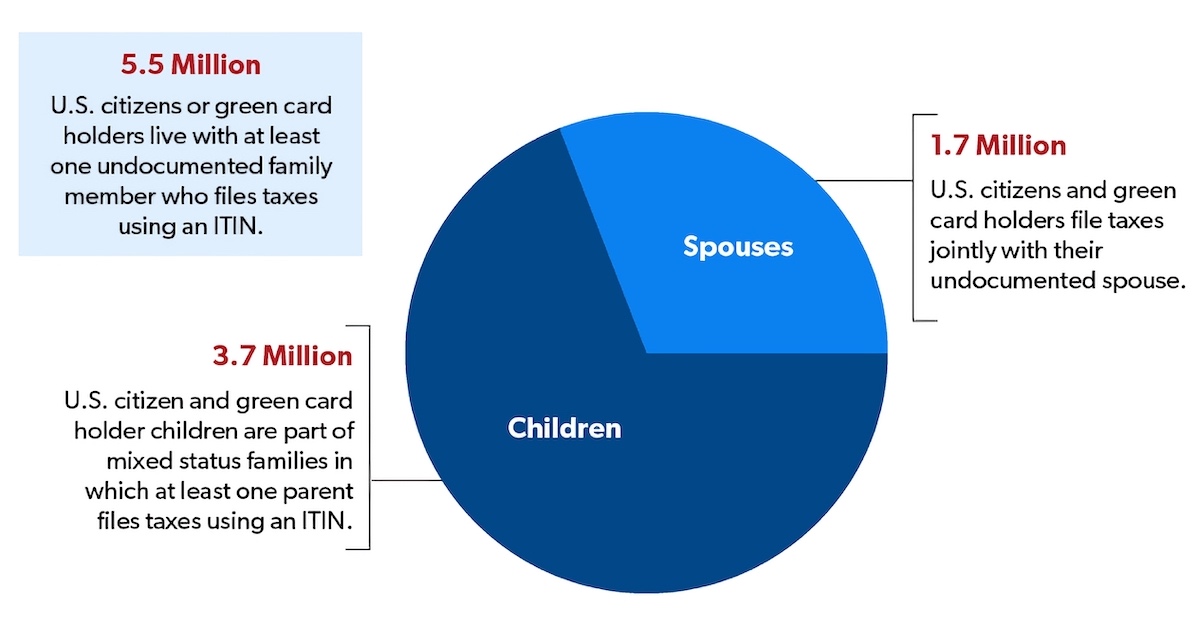
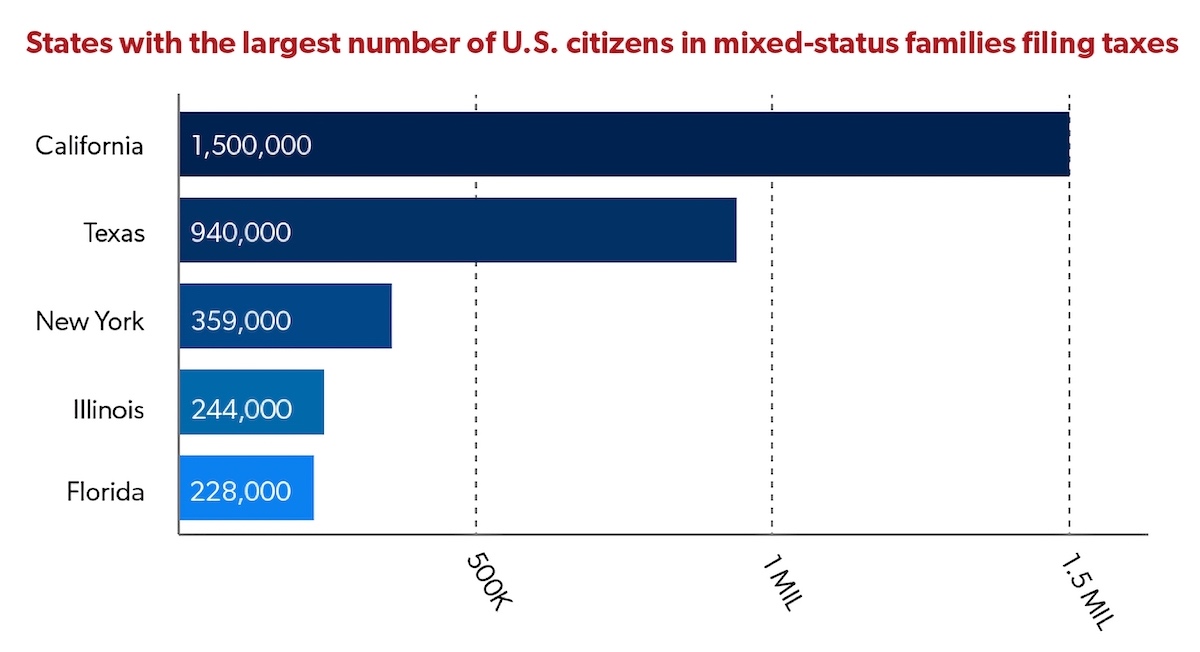
According to the National Immigration Law Center, “a mixed-status family is a family whose members include people with different citizenship or immigration statuses. One example of a mixed-status family is one in which the parents are undocumented, and the children are U.S. born citizens”. The state of California has the largest number of U.S. citizens in mixed status families filing taxes, at 1.5 million people. This is a topic I would like to bring more attention to because many people may come from or know someone from a mixed status family, this includes students at USC and clients seen during fieldwork or residency, and this may not be something that is often brought up in the classroom. Personally, I live in a mixed status family, which includes DACA recipients and people without any documentation, with some extended family having other statuses as well.
Source: Migration Policy Institute, “Mixed-Status Families Ineligible for CARES Act Federal Pandemic Stimulus Checks” (May 2020), migrationpolicy.org/content/mixed-status-families-ineligible-pandemic-stimulus-checks
Source: Migration Policy Institute, “Vulnerable to COVID-19 and in Frontline Jobs, Immigrants Are Mostly Shut Out of U.S. Relief” (April 24, 2020) migrationpolicy.org/article/covid19-immigrants-shut-out-federal-relief
This past year has been really tough financially for my family and me. The multiple stimulus packages that were passed came with a lot of limitations for mixed status families. For example, as a USC student who is undocumented with DACA status, I was unable to apply to the CARES Act financial assistance for college students. After doing some research and waiting for the final relief bills to be amended and passed, I was fortunate to receive the stimulus check because I have a temporary work permit via DACA. However, not all undocumented students are DACA recipients, and many undocumented people did not qualify for anything, even though they pay taxes every year with an Individual Taxpayer Identification Number (ITIN) number. In the last year, I saw many people be excluded from federal assistance simply because of their immigration status, personally at home, with friends, and at residency. My parents and many of my clients in primary care were impacted by the exclusions in the COVID-19 relief bills, including the most recent under the Biden administration.
During this time, many families continue to rely on food banks, are behind on rent, and are surviving on the little help they can get. For example, I helped my parents and some of my clients apply to local and state specific relief programs which provided some financial assistance, but not nearly enough. And for many it’s not an easy process due to technology access, literacy levels, social support, etc. Last fall, I helped my parents write a letter and email it to a rent relief program that provided $500. I was appreciative that non-profit organizations and certain school departments took it upon themselves to be more inclusive and provide some type of financial assistance for students that may have not qualified for the CARES Act. As a current student, I was able to apply for the USC Ostrow Emergency Fund, the USC Graduate Student Government Emergency Assistance, and Immigranted (non-profit organization) for financial assistance to get through the year. Most of that assistance and my stimulus checks went to home expenses that my parents were simply unable to cover.
I believe this is an important discussion we need to have or at least consider in the academic setting and occupational therapy world. As I stated earlier, this impacts students at USC and in the OT programs, as well as clients being seen by occupational therapists/residents and/or fieldwork students. It’s important to consider how students may be navigating their own experience within a mixed-status family or perhaps have family/friends, clients, or colleagues that are experiencing this. As the Chan Division continues to push for more diversity and students from different backgrounds come in, it’s important to consider how prepared we are to support their education and clinical experience within the context discussed above.
No matter your political views, from an occupational therapy lens, we all have a responsibility to promote occupational engagement and occupational justice. This may include supporting clients navigating access to resources. As I found myself doing with my family and clients in primary care, I was that person that supported their own resource seeking as a means for survival during the pandemic. The reality is that not everyone has access to OT services or a family member who can help them seek resources. This is a very complex topic and there are many layers to it, perhaps many terms you may not be familiar with. I am always available for any questions (.(JavaScript must be enabled to view this email address)). I ask you to be open minded and encourage you to have these uncomfortable conversations. It is never too late to start learning and getting involved in the discussion. The COVID-19 pandemic revealed and exacerbated many of the disparities and social inequalities that have been there for many people in the United States, especially the undocumented population. I want to leave you with the questions below to reflect on:
- As a current or future occupational therapist, how are you going to support clients experiencing occupational injustices due to their immigration status?
- How are the needs of students within mixed-status families being met? How can we best support them in reaching their educational and professional goals?
References
Chishti, M., & Bolter, J. (2020, December 11). Vulnerable to COVID-19 and in Frontline Jobs, Immigrants Are Mostly Shut Out of U.S. Relief. Migrationpolicy.Org. https://migrationpolicy.org/article/covid19-immigrants-shut-out-federal-relief
Fact Sheet: Mixed Status Families and COVID-19 Economic Relief. (2020, August 13). National Immigration Forum. https://immigrationforum.org/article/mixed-status-families-and-covid-19-economic-relief
Mixed-Status Families Ineligible for CARES Act Federal Pandemic Stimulus Checks. (2020, December 9). Migrationpolicy.Org. https://migrationpolicy.org/content/mixed-status-families-ineligible-pandemic-stimulus-checks
The Affordable Care Act & Mixed-Status Families. (2017, October 20). National Immigration Law Center. https://nilc.org/issues/health-care/aca_mixedstatusfams
⋯

You Don’t Need to Be Perfect, You’re Still Learning ⟩
March 1, 2021, by Daniel
Admissions Classes Fieldwork Life Hacks
Over the last couple of weeks, I have been talking to students that find themselves at different points in their OT journey. This is a busy time as many wait for updates from admissions, some still deciding whether to pursue the OTD, and others wondering what field of OT to pursue as they find themselves in the final year of their program. Being able to connect with students from different backgrounds is my favorite part of this position and it is a privilege to learn all your stories. Around this time in 2018, I was waitlisted for the Entry-Level Master’s program, and to be honest I did not have high hopes that I would get in because of my GRE scores. At the same time, I was working a lot and still trying to finish my Bachelor’s degree while struggling to do well in Chemistry (I know, what a fun last semester!). When I have these conversations with students it takes me back to these days, the good and the bad times. This is a time in my life when I thought I had to be perfect in order to be successful. Whether you are waitlisted, deciding on an OT program, just discovering OT and not knowing if this is the right choice or feeling overwhelmed with the overload of information coming at you, remember that you are not perfect. None of us are.
Make sure you are taking the time to breathe and engage in things you love to do, even if it’s a few minutes of your day. Take those minutes to spend it with loved ones, call someone, and eat! Remember to practice what we preach and try to find a balance. You cannot control everything, so focus on the things you can and take care of yourself. We want you to be at your best during class, when studying, at fieldwork, and with clients. You should always strive to give it your best, but it’s okay to not be perfect. When you know you gave it your best despite the circumstances, I believe you can be at peace with the results. This way of thinking and restructuring my thoughts has helped me cope with the demands of grad school. Remember that part of learning is to fail and try it again. Dwelling on it will not change anything, but what you can do is learn from those shortcomings. Maybe you had a practical that didn’t go as planned, perhaps a rough fieldwork or residency day, you know, it happens! And often those are the times that stay with you the most, when you make a mistake, when you failed at something, or when you didn’t know what to do.
I recently read a quote from my assigned class reading about an immigrant woman that says, “I may not remember everything I have learned, but it has made me who I am today”. This is the quote I needed last week as I found myself struggling through my busy days. The long days and nights, assignment deadlines that feel impossible to meet, back-to-back meetings, the endless information introduced every week, etc. At times, it may feel like you’re just on autopilot, going through the motions. We can get so caught up in not knowing enough for an upcoming exam, for fieldwork, or for your residency setting. And of course, I do not know every single thing that was ever taught to me in school, but I have learned lessons from it all along the way. The Master’s program and now the OTD program, they have both challenged me in different ways. They have both made me question my abilities and have tested my motivation.
If you are reading this now and find yourself with doubts about what to do next, remember that you don’t need to be perfect. As you proceed to the next step in your journey, remind yourself that perfection is an unrealistic expectation that should not be put on anyone, you are a person and student that is still LEARNING. Take the necessary steps to learn from the particular experience you find yourself in, and with a little perseverance just keep going. Use the resources available to you, reach out for help, and don’t ever be afraid to ask questions. Lastly my virtual door is always open for those that may relate to this notion of perfection or if you have questions about OT and higher education (.(JavaScript must be enabled to view this email address)). I also invite you to make comments below if you would like 😊
⋯

Electives During the OTD Program ⟩
February 5, 2021, by Daniel
This Fall I was feeling burnt out towards the end of the semester. It was my first OTD semester with classes being virtual and it was my first time being the only OT at my site (primary care clinic). Many times, I was just trying to keep up with my assignments and residency demands. During the month of October, I began looking at what classes I would be taking for the Spring semester, but it was all just too stressful, and I kept pushing it back. My bi-weekly check ins with my faculty mentor and clinical preceptor helped with brainstorming ideas for potential electives to take in the Spring. The idea of getting to choose courses that interest me and plan my own schedule sounded refreshing. I began to look for electives outside of the OT department since I’ve never had the opportunity to take a class in another department.
Taking the advice from my check ins and further understanding the needs of my residency population, I decided to look for electives in gerontology, policy, and pain medicine under the Keck School of Medicine. Eventually, I came across several exciting opportunities to take as electives but not enough units because of the 2 additional elective units I took during the Master’s program. Remember that during the OTD program you can take 4 units of electives (unless you took extra elective units as a USC Master’s student). For students starting their OTD in the fall, in the Spring semester you will also be taking OT 621: Occupational Therapy Leadership: Contemporary Issues (4 units).
Since the beginning of my residency training our focus has been supporting clients with uncontrolled diabetes and hypertension. I also had the opportunity to provide short consultations, with one of the highest requests being for chronic pain. Clients on our active caseload will often request support with pain management as well due to diabetes complications such as neuropathy and other comorbidities that cause pain, making it harder for them to engage in their health management and daily occupations. Given this need and while doing further research, I decided I wanted to use my 2 elective units to learn more about pain and better support my clients. After reaching out to Keck faculty to get clearance for pain medicine courses, I enrolled in PAIN-704: Pain and Society: Epidemiology and Cultural Issues and PAIN-720: Physical and Occupational Therapies. PAIN 704 is a course focused on exploring societal issues related to pain and pain management such as culture, ethnicity, caregiving, social and psychological factors. PAIN 720 is a course focused on discussing different OT and PT techniques to assess and treat chronic pain.
The first week of January I had a check-in with Dr. Sarah Bream, our OTD Program Director. During our meeting I shared with her my desire to take MDED-511: Immigrants, Illness, and Narrative Medicine (4 units), but not having enough units. MDED 511 is a course that examines immigrant experiences in the U.S. through the lens of narrative medicine, aimed to deepen students’ understanding of critical issues affecting immigrants in the U.S. and develop skills to better serve immigrant communities and populations in healthcare and other social services. I shared with her my passion to increase my knowledge and skills to better serve immigrant communities during my residency and in my career. Dr. Bream was very receptive of my ideas and even provided additional advice to work on for my OTD portfolio. She shared with me that on a case-to-case basis, exceptions could be made to substitute OT 621 with another course. I was really surprised but excited to hear this because that meant I could take the MDED 511 course. I truly appreciated her help with problem solving, finding a way to shape my OTD experience, and taking care of the necessary paperwork to make the change.
I am now three weeks into my Spring semester, and I am feeling refreshed (after Winter Break), more confident in my clinical skills, and looking forward to my electives expanding my knowledge. I wanted to share my experience choosing electives during the OTD because if you are feeling unsure about what to take or simply don’t have enough units to take certain courses, I encourage you to reach out to Dr. Bream, your faculty mentor, classmates, the student ambassadors, or even former students because unless you ask, you may not know about the different ways that you can customize your learning experience.
⋯