OT in Oncology

February 15, 2018
by Kaitlyn
Getting Involved What are OS/OT?
I have met a lot of amazing and inspiring people during my journey to becoming an occupational therapist. While I try to preach equality as much as I can, there is still one patient that remains one of my favorites to this day. In my freshman year of college, I volunteered at USC Norris Comprehensive Cancer Center, where I met the woman who would spark my road to health care.
Without going into too much detail, she was the kind of woman who wore lipstick everyday even though symptoms and side effects of her diagnosis and treatment yielded a thinning (and nearly disappearance) of her lips. She told me countless stories about her life in her twenties and early thirties — all of places she had lived, all of the countries she had traveled to, and all of the men she had to date before she found her husband (this is my mini plug to say happy belated Valentine’s day!). She was such a light in my life at the time (and still is, to be quite honest) and my interactions with her and all of the other patients in that hospital are what solidified that working with patients in healthcare is what I wanted to do for the rest of my life.

Golden hour outside City of Hope.
That was nearly 7 years ago (wow, how time seriously and flies!), and since then, oncology has always held a special place in my heart. As I continued OT school, I was so happy to discover that OT does play a role in cancer care as well. With that being said, a few weekends ago I attended the ‘OT in Oncology Symposium’ hosted by OTAC and City of Hope. This is the first time they’ve held an event like this on this topic, so I knew that I could not pass up the opportunity.
At this event I learned about a multi-pronged approach to cancer-related fatigue, pediatric oncologic OT in acute care, a comprehensive approach to address cancer-related cognitive impairments, evaluation and treatment of of chemotherapy-induced peripheral neuropathy, psychosocial interventions across the continuum of cancer care, and even how to manage cancer as a chronic condition using a Lifestyle Redesign® approach (lectured by our very own, Dr. Camille Dieterle).
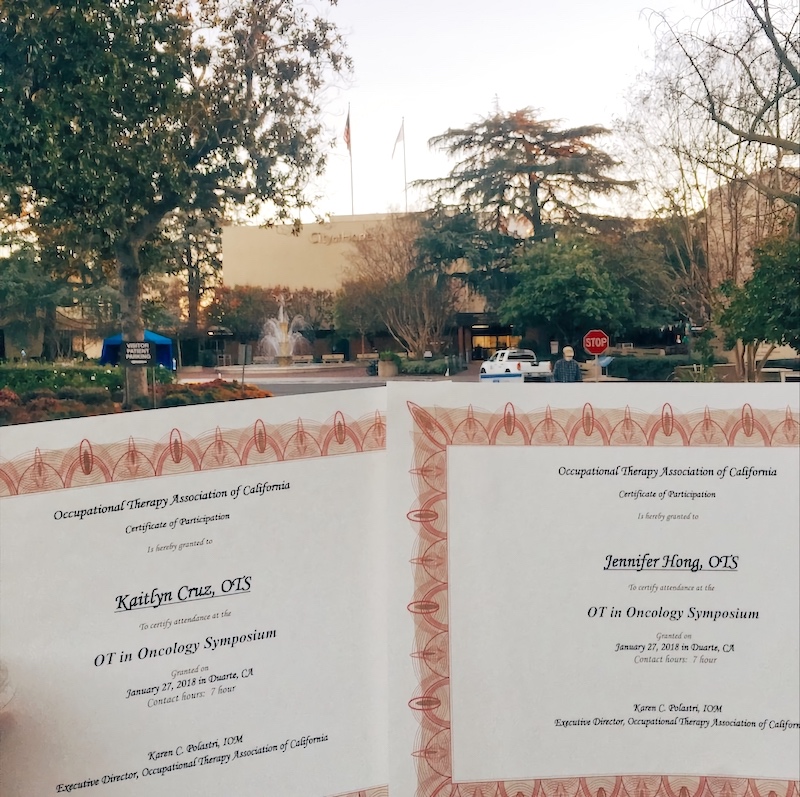
Symposiums are always fun with a friend! I went with Jen, a friend of mine who is also in the program.
Within these topics, I learned about how fatigue, as a result from cancer, can negatively affect cognition in patients’ everyday lives and how we, for example, can educate the client on how to take proper rest breaks throughout the day. I also learned about the importance of facilitating normalcy and encouraging toddlers with cancer to participate in play in order to yield a sense of autonomy and self, even in a setting like a children’s hospital. In addition, I learned different exercises (i.e., median nerve glides, overhead elbow active range of motion stretches, etc.) to incorporate into treatment sessions with patients to help reduce edema (swelling) and increase tissue circulation in the body. I learned a lot more but if I kept on going this blog post would be way too long!

Outside City of Hope, there are trees you can attach written notes on. A lot of the notes had messages of hopes, wishes, and desires for loved ones.
One of the biggest takeaways I learned from this symposium is that in oncology care (and in any area, really), an extremely essential role for OTs is to present and instill hope in our patients. Yes, as OTs we assess and work on patients’ instrumental activities of daily living (IADLs), activities of daily living (ADLs), and range of motion (ROM), but an even more important role is that we aim to make our patients feel understood and really look at what roles are most impacted during this time in their lives. A role can be that of a mother who wants to be able to pick up her child, or it can even just be that of a woman who wants to be able to put lipstick on every day.

⋯
Next by tag Getting Involved ⟩ What are OS/OT? ⟩
⋯





