Student Blog
Rashelle

Faculty Mixers! ⟩
December 1, 2015, by Rashelle
Community Getting Involved School/Life Balance
This year for the annual faculty/student mixer series, students were invited to partake in fun events organized by our student council professional development chairs. I was fortunate enough to be available to attend all three of them this year!

Bowling with Faculty
At the first mixer I got the opportunity to show off my (un)impressive bowling skills with Dr. Myka Persson, a previous professor, Carey Sokol, my past fieldwork coordinator, and Amber Bennett, who coordinated the Career Fair, which I attended the day after. It was awesome to see faculty members in such a fun, informal environment, which really allowed me to get to know them apart from the structured school work and meetings.

Urth Caffe with Faculty
The second faculty/student mixer was held at Urth caffe with Dr. Karrie Kingsley, one of my favorite professors, along with Dr. Tracy Jalaba and Dr. Lindsey Reeves, who recently completed their doctorate degrees at USC’s distinguished Faculty Practice. It was an honor to sit next to them over dinner, and to hear about their captivating journies of how they got to where they are today.

Barbara’s Brewery with Faculty
Lastly, after my final day of fieldwork at the Keck Hospital of USC, I got to celebrate it with, coincidentally, my fieldwork supervisors! Dr. John Margetis and Dr. Kim Lenington are two of USC’s finest clinical faculty, who taught me the ins and outs of how to intensely care for patients in an intensive care unit. If that was too cheesey, it must be from where my mind has drifted after all of those nachos we ate!
These intimate gatherings truly made me feel welcomed into the Trojan Family. Not only will I feel less intimidated when approaching these faculty members in the future, but also I was able to connect with first year students, who may have been intimidated by me! Every day, with every new person I meet, I see how large this network of Trojans is, and how supportive and encouraging they can be as we go through this journey together.
⋯

Wheelchair Mobility Creating Real Accessibility ⟩
November 22, 2015, by Rashelle
As an occupational therapist, we may have the opportunity to order wheelchairs for people after completing a thorough evaluation of them. When deciding what type of wheelchair to order, we analyze a person’s engagement in activities, current abilities, and desires for mobility. We also provide education to clients on how to best utilize their wheelchair in order to maximize their participation in daily activities (e.g., home and community mobility). Last week, we were fortunate enough to receive a lesson from an expert wheel chair maneuverer.

He taught us how to pop epic “wheelies” to get over road bumps, how to conserve energy while going up ramps, and how to courageously (yet safely!) back up over curbs.

These lessons not only taught me basic techniques, but also the immensity of strength needed, both physically and mentally, to successfully overcome barriers of accessibility. It was inspiring to say the least, to hear about our guest speaker’s involvement in a nationally competitive wheelchair rugby team, living perfectly on his own, and even driving himself away in his inconspicuous, yet highly adapted car. The individuals that are able to master wheelchair mobility, in order to live independently and happily, are the true superstars of society!
⋯

Learning How To Dress in OT School! ⟩
November 10, 2015, by Rashelle
In OT 502: Adult Physical Rehabilitation, we have a lab every week to learn practical skills that we can incorporate when treating patients — this week depicted below, focused on the activity of dressing.

Sock Aid and Dressing Sticks
The picture on the left demonstrates me using a sock aid! This assistive device is often utilized with adults, who have physical limitations that make dressing difficult. The sock aid can facilitate modified, independent dressing for people following surgeries to the hip, spine or legs, or for those who may live with chronic diseases such as arthritis, multiple sclerosis or Parkinson’s disease. Within that same lab, we learned about the benefits of dressing sticks, button hooks and reachers to assist with upper body dressing (as pictured on the right).
Additionally, in my level 1 fieldwork rotation, I learned how to dress a patient with compression bandages, in order to treat edema. Edema is a condition in which a person has a fluid buildup in a part of their body. By dressing patients with these bandages about once a week, the fluid can drain away from the swollen region.

Edema Bandaging
(That’s my foot! I even got the real patient experience by having to lay in the hospital bed).
Furthermore, while you can learn these patient dressing techniques at most occupational therapy schools — USC also teaches students how to dress professionally and with school spirit!

Joe and Ellen Dressing Professionally
Here, Joe Ungco, a fellow student ambassador, and Ellen Wleklinski, an OTD resident are modeling their business attire, which we wear often for class presentations, fieldwork, conferences, meetings or interviews.

USC tailgate outfits
Finally, we FIGHT ON proudly with our traditional USC attire for football games, tailgates and other sporting events.
⋯

Assessing Cognition While COOKING! ⟩
October 24, 2015, by Rashelle
This week, in the Primary Care Elective class, we learned how to assess somebody’s cognitive abilities, by analyzing their performance in the kitchen! To begin, we looked at the Kitchen Task Assessment, which requires a patient to prepare pudding by following the directions of a commercial package. I was able to role play as the patient in front of the class, as another student pretended to be my therapist. Due to my limited knowledge in cooking and safety awareness, I fulfilled the perfect role of a patient needing cognitive support during a functional task of daily living.
The picture below displays the score I got on the Kitchen Task Assessment.
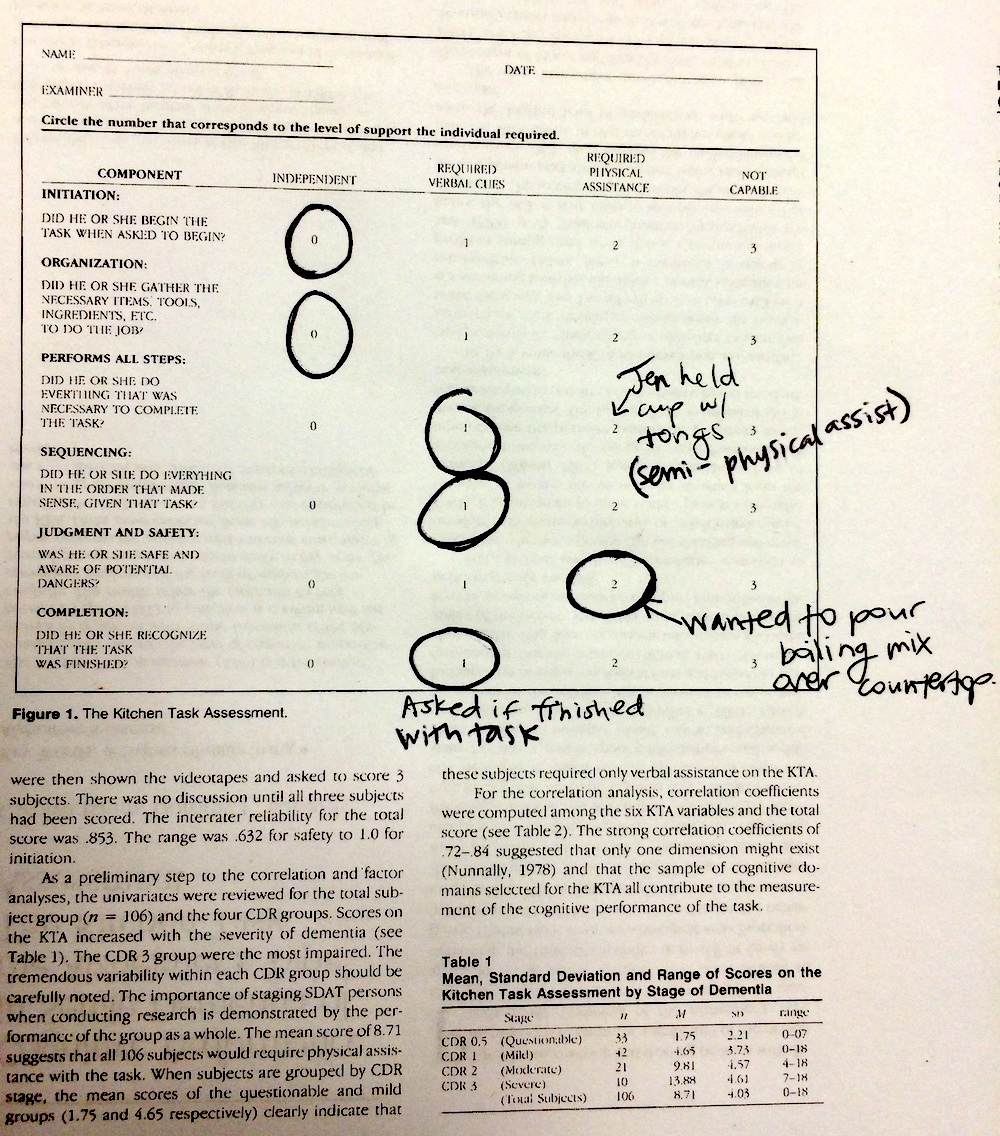
Scoring the Kitchen Task Assessment
As you can see, I required assistance from my therapist both in verbal cues and physical assistance. Jen, the practicing therapist, needed to give me verbal reminders of when to add in the pudding mix to the boiling water, how many cups were needed to pour the finished pudding into, and when the task had come to a complete end. I required slight physical assistance when Jen held one of the cups for me to pour the pudding into, and when I attempted to pour the boiling hot pudding mix into the cups on the counter, in an unsafe manner. PHEW. Was it a relief when I finished!

Finished Pudding After Completion of Kitchen Task
Every step of the pudding-making process we, as a class, discussed possible scenarios that we may encounter when working with a patient that may have an actual cognitive impairment (e.g., when diagnosed with Alzheimer’s or a traumatic brain injury). After role-playing this encounter, I can better empathize with my future patients, whom may face confusion, agitation, disappointment, apprehension or timidness while performing this task. I am excited to also be able to problem-solve with these patients on how they can change their approach to the task, to be able to cook as independently as possible, in a safe and effective manner.

Kettle Test
Here, two other students, Kellyn Trummer and Renée Boivin, are demonstrating the Kettle Test — a cognitive functional screening test that requires a patient to prepare two cups of hot beverages. Similarly to the Kitchen Task Assessment, every component of the task is scored on the patient’s level of independence, which the therapist then will use to determine the amount of assistance the patient will need tp perform a functional task. For instance, the Kettle Test analyzes a person’s ability to prepare the hot water, assemble the kettle and add all of the ingredients together despite having visual distractions.
Overall, this lesson was a great opportunity to improve our clinical reasoning skills, and to practice assessments that an occupational therapist may use in the future!
⋯

The Fault in Our Stars Creates the Perfect Alignment of Health Care Collaboration ⟩
October 15, 2015, by Rashelle
Getting Involved What are OS/OT?
As mentioned in my post before, one of the most unique things about USC is the opportunity to learn from an interdisciplinary team. This week I went to a movie screening of The Fault in Our Stars at the USC Norris Comprehensive Cancer Center. After the movie viewing there was an interdisciplinary panel led by the Norris Medical Library, consisting of a Medical Doctor (MD), Registered Nurse (RN), Physical Therapist (PT) and Occupational Therapist (OT), whom all have had experience working with adolescent and young adults (AYA) diagnosed with cancer.

These health professionals answered questions regarding the movie, shared myth busters, elaborated upon roles of the hospital staff in the movie, and described the lessons they’ve learned from their firsthand experiences working with this population. The USC faculty and staff also spoke about the differences in treatment approaches when working with AYA, in comparison to children or older adults. This section of the discussion hit home for me in particular, due to my passion for working with AYA in their difficult transitions acquiring new roles and forming individual identities. While the movie itself turned on a faucet of emotions and tears, the panel afterward taught me how to cope with the emotional hardships that may come with working so closely with AYA diagnosed with cancer. This heartwarming, encouraging and uplifting event demonstrated the capcity of each profession to distinctively contribute to the alignment of the stars, in order to facilitate the greatest recovery for all patients.

Caryn Roach and OT Students
Here is a picture of a few occupational therapy students surrounding Dr. Caryn Roach, the occupational therapy representative in the panel. How occupational therapists contribute in particular to this health care team, is by ensuring that each patient is able to participate, to their fullest capacity, in activities that are meaningful to them — may it be reading a book, feeding themselves, showering independently, socializing with their friends or traveling to Amsterdam with a significant other to meet one’s favorite author, Van Houten — occupational therapists find the supports, educate patients on adaptive devices, implement energy conservation techniques, strengthen muscles and increase ranges of motion to provide a greater range of accessibiility and quality of life for the patient.
⋯





