Student Blog
Classes
What I Learned in a Week as a Medical Volunteer in Panama ⟩
December 13, 2024, by Guest Author
Classes Community Diversity Getting Involved International
By Carly Martinez OTR/L, USC Chan Post-Professional OTD student

Carly Martinez OTR/L
When you read the name of the country Panama, what comes to mind? If you’re anything like me until about a month ago, your knowledge consists solely of the famed Panama Canal. After spending 8 days there as a medical volunteer, I won’t pretend to be an expert, but I can give you a brief glimpse into my journey.
During the first semester of my post-professional OTD, I decided I would take what I thought would be my final elective, MEDS 577, Global Palliative Care with Dr. Ben LaBrot. It felt significant for me as a practitioner because I had learned a little bit about hospice and palliative care through my master’s program at USC, and knew that occupational therapy (OT) had a role to play in that area. At the same time, it still felt like we had only skimmed the surface. Through that course, I learned a lot about autonomy and dignity, values my professional OT education had espoused, however, this was a deeper dive into this particular context.
A few weeks into the course, Dr. LaBrot shared that he would have to record class since he would be in Panama. After class the following week, some students stayed after class to ask the professor about another course he taught. While unintentionally eavesdropping, I learned that he was the founder of a medical volunteering organization, Floating Doctors, based out of Panama. Excited at the possibility of going abroad again as part of my OT education, I asked if his program accepted occupational therapists. He was enthusiastic about my participation and clearly an ally of occupational therapy through what he shared in the curriculum. It would count as my final elective, and I could get credit for volunteering through MEDS 554.

Volunteers for the week including physicians, a veterinarian, a dentist, medical students, and one OT.
Months later, I would find myself in a rainforest, translating for a classmate who graduated from medical school in Indonesia, learning how best to explain things to individuals who grew up in a completely different context than myself. Floating Doctors works with the members of the Ngäbe, an indigenous population in the Bocas Del Toro province of Panama. This region is designated as part of the Ngäbe-Buglé comarca, an officially recognized province that is part of how the nation is divided, similar to statehood, which allows for self-governance among the indigenous population. To get there, I flew from LAX to Panama City, then travelled to a second, smaller airport in Panama City to fly to Bocas del Toro, an island in the northern archipelago region of the country.

Preparing to land in Bocas del Toro
During clinic, we slept outdoors in the rancho where we provided services in hammocks strung from metal beams and bathed in the river, as do the community members. However, I will say that it was not the most rugged camping experience of my life. We had indoor plumbing, could purchase wifi from a nearby home, and had meals cooked for us by local women. Patients brought goods to sell, like the best chicken empanadas I’ve ever tasted, sizable chicken tamales wrapped in banana leaves, and artisanal breads. Some families told me they walked for a day through the mountainous terrain to be seen by the doctors. Did I mention that the weather hovered around 90 degrees and 100% humidity? The patients came well-dressed, with women in nice dresses and men in polos and jeans. I got the feeling they were dressed up to see us, but also because they would be seen by many other people who were also attending the clinic.

Preparing for a day of clinic. Folks were lined up before we arrived.

A visitor to the clinic wearing a traditionally-adorned dress (photo taken with permission).

Enjoying refreshments (with ice!) with other volunteers in Bocas after a successful week of clinic.
Visitors to the clinic generally fall into two categories: fast lane or chronic. Fast lane is for new or relatively simple cases, such as needing paracetamol to manage fever, albendazole for concerns about parasites, or birth control injections. Chronic patients are seen every three months, as the team returns to each site regularly, cycling through the 28 sites they service. Though the providers change, there is still consistent care for diabetes, hypertension, and asthma, to name a few of the more common conditions. Patients can have their names put on a list for a doctor who comes by to perform cataract surgery as part of another program. Referrals can also be given in cases where a patient requires more or specialist care, such as the case of a 6-year-old girl who seemed to be struggling in school, based on her mother’s description. Though I did an informal writing assessment, she would need more testing to determine if she was reaching developmental milestones, something the organization is not equipped to offer at this time.
To be seen by specialist medical providers, they would need to go to a major town nearby. Although this community had a medical clinic nearby, the resources there were limited. Travel to David, a town with more medical resources, would require a bus ticket and potentially a stay in the city, a prohibitively expensive expenditure for some of the patients. Boquete is closer, though it is not as well-resourced and still requires a bus ticket to get through the mountains on rocky dirt roads, which do not have lights, limiting travel for safety reasons.
This trip felt challenging to my professional identity. As a new practitioner, I worry about the role OT can play in different contexts. The lead medical provider for the week was not familiar with OT, or Ergotherapy as it is often referred to in Europe. He told me that this does not exist in his home country of Russia. The World Federation of OT only credentialed the University of Panama’s OT program last year, in 2023. I wondered about the relevance of the profession to people whose activities of daily living (ADLs) likely consist of more life-sustaining occupations than mine do, such as gathering water or washing clothes by smacking them against rocks in the river, in addition to household management tasks like washing dishes and cleaning the house.
I could see the applications of OT for those who worked cutting bananas, as they suffer from repetitive motion injuries, for children in school, and likely, for individuals with mental health concerns, if I were to speculate. However, I also acknowledge that I don’t really know much about their everyday lives because I didn’t have the opportunity to get to know them in the ways that would be necessary for an OT evaluation. I longed to know more about what an average day is like, as this would allow me to begin imagining what role occupational science (OS) could play in trying to understand what life is like for the Ngäbe. If OS has taught me anything, it is that I am not an expert on the culture of the Ngäbe. In order to work with a population in a way that garners buy-in, one has to try to understand the values to support what is important to their patients.
All of this is not to paint a picture of an area with fewer resources; after all, there are rural areas of the US with limited access to hospitals or routine medical care. Instead, I hope that Panama provides opportunities for OT and OS to continue to develop in multiple contexts, ranging from the traditional academic experiences OT graduates may have in the larger metropolitan areas, to the volunteer OT services with Floating Doctors, as well as others yet to come.
For my final occupational therapy doctorate (OTD) project, I created a set of OT practice guidelines or a white paper, in support of the development of OT services for Floating Doctors. The hope is that this will allow for the expansion of OT services within the organization, encouraging more OT volunteers to attend, and familiarize the individual medical providers with the scope and potential interventions OT can provide. It will also be part of the information Floating Doctors provides the Panamanian government to continue its services there.
⋯

Day In the Life of an Undergraduate BS-OTD Student Vlog ⟩
December 10, 2024, by Avery
Classes Community Getting Involved Living in LA School/Life Balance Videos
Join me as I take you through what a typical day looks like as an undergraduate student in USC Chan’s accelerated Bachelor’s to Doctorate program in Occupational Therapy! One of the things I love most about this program is the balance it allows me to strike between my occupational therapy (OT) courses, engaging electives, general education classes, extracurriculars, and free time.
From participating in enriching clubs and student organizations to spending quality time with friends and exploring the vibrant city of Los Angeles, I’m able to enjoy a well-rounded college experience while still focusing on my OT studies.
As always, if you have any questions about the BS-OTD program from an undergraduate perspective, feel free to reach out!
⋯

My OS Minor Recommendations ⟩
November 13, 2024, by Cara
Classes Life Hacks School/Life Balance
Spring course registration is already underway, and if you’re still on the hunt for classes to fill up your schedule, you’ve come to the right place! Whether you’re considering a minor in OT or just looking to create a healthier and happier lifestyle for yourself — here are my recommendations.
OT 101: Caring for Your Self: Engaging in Healthy Habits and Routines
OT 101 is all about YOU! This course helps you learn about self-care practices to incorporate in your everyday life, like mindfulness, setting goals, and time management. Throughout the course, I was paired up with another student for weekly meetings where we reflected on our self-care experiences and feelings. Sometimes we did activities together, like yoga, drawing our breath art, or eating. It was a great experience that helped me improve self-awareness and also built a lasting friendship. Since taking this class, I’ve realized how self-care is not a luxury — it’s a necessity for overall wellness. I’ve noticed improvements in my productivity, calm mindedness, and greater self-acceptance by making time for myself. College can often feel like an endless race where we neglect our health and personal needs, but taking time for self-care can make all the difference.

Me and my partner, Mahalia, doing yoga!
OT 251: Across the Lifespan: Occupations, Health, and Disability
In OT 251, I learned about how people grow and change as they go through life and how this affects the activities they find meaningful. We explored human development by looking at different factors like biology, psychology, society, and culture, and how these all connect to shape what people are interested in and value in their lives.
What made this class really fun was the emphasis on building a positive and engaging learning community through peer learning. I often worked in groups on case studies, role-played different stages of development, and did discussions where my group mates and I reflected on our development and how it affects what we do. I really connected with my peers through both our shared experiences and differences, deriving new insights on how development is nuanced. And I still keep in touch with them to this day!
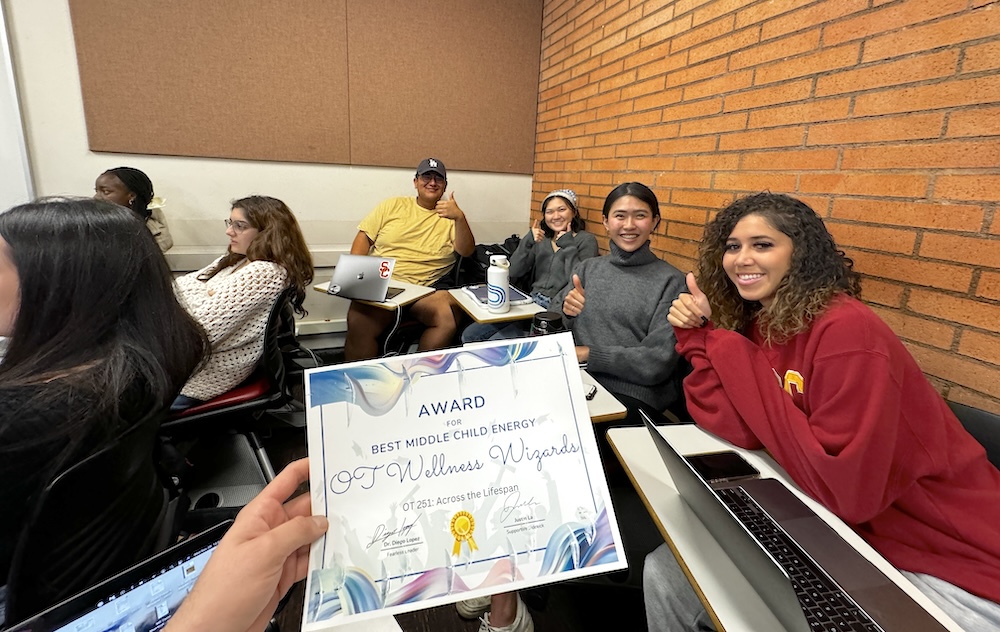
At the end of the semester, my group and I, called the “OT Wellness Wizards,” received the award for “Middle Child Energy.”
OT 340: Animal and Human Interconnection in Daily Life
If you love animals, OT 340 is a must! This course explores the relationship between humans and animals. I learned about K9s, therapy dogs, foster animals, among many others. Occasionally, some furry friends came to visit too. As part of the course curriculum, I spent 8 hours interacting with animals to further understand how humans and animals affect one another. I volunteered at a local shelter, walking German Shepherds for two hours each week. The experience was rewarding, teaching me about humility, compassion, and loyalty. I also found it amazing how animals still love us no matter how we treat them, and continue to persevere to live a better life than before. If that doesn’t convince you, I don’t know what will!


These courses are just a taste of what the OS minor has to offer, and I encourage you to consider them as you finalize your spring schedule. They will deepen your understanding of both yourself and others while providing practical skills you can apply in your everyday life. Check out our other OS courses here!
⋯
Taking my first exam, more than a decade later ⟩
November 12, 2024, by Tanya
Beginnings and Endings Classes International
The anxiety that hit me on the morning of my first exam in a long time was one I had not experienced, one that felt so foreign. Perhaps it is because I was not used to it as it has been a while, and not to sound dramatic but it felt worse than going for a job interview or presenting in front of a large audience. Everything felt so uncertain and unexpected, and I, as a person who valued control and preparedness, felt quite lost and nervous.
Even the platform that the exam was on seemed foreign, with the entire exam being digitalized. This is a stark contrast from the days when my biggest worry was that I had multiple sharpened 2B pencils to shade the correct option in a multiple-choice exam. I was amazed that the paper could be downloaded before the commencement of the exam, and the exam software came with tools such as the highlighter and timer visible on your screen.
I was overcome with a sense of relief mixed with anticipation of how I performed once I saw the green screen notifying me that the submission was successful on my screen.
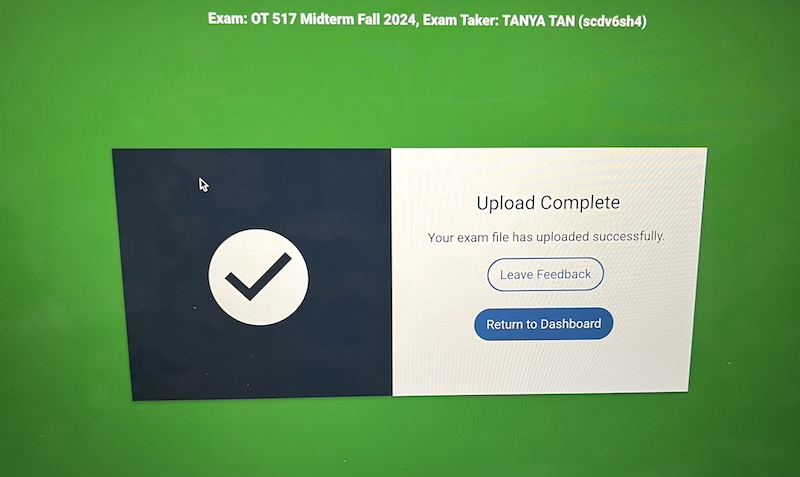
After my first Sensory Integration mid-term exam — taken with permission from Dr. Gunter upon submission
Given the option, I would have much preferred to have written a paper instead, as this would have allowed me to weave in my thoughts and opinions supported by evidence. When I reflected on the entire experience, I would say my anxiety stemmed from the unfamiliarity of the advancement in technology as well as the entire examination process that felt so foreign rather than the actual content. And this was yet another way for me to learn how to adapt to changes and move with the times.
If you have not been on the academic journey for some time, here is what I did to help deal with these changes. It did not remove the nerves completely, but it helped me settle into it faster.
1. Having stationaries that help with note-taking
If you are like me and prefer to organize and write down notes on paper to visualize the information learned, it will be helpful to bring some writing implements or sticky notes that you are used to back home.
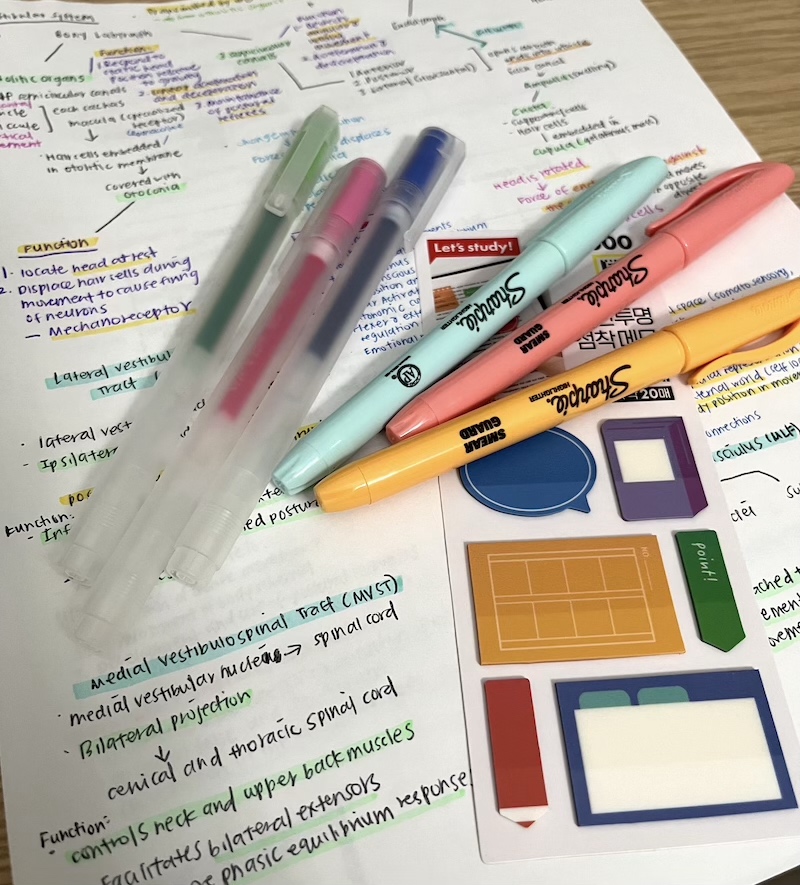
Some of my writing implements that I brought over from Singapore
2. Follow your usual sleep pattern
Hearing some of my classmates share about the later times they sleep and how they feel more efficient or productive, made me consider this choice and attempt it. I usually head to bed by around 11 pm and decided to try staying up till 1 am. Sad to say, this was counterproductive, and I was less efficient and felt even more lethargic over the next 2 days. Know your body system and do what is best for you, you do not have to change your routines despite adopting a new role.
3. Enjoy leisure amidst the exams and assignments
Along with midterms also come assignment submissions, this can be a lot, and you may feel overwhelmed by it. It may feel that every minute should be channeled to studying or reading another article, however, engaging in leisure does clear your mind and refreshes you. It is the little things that can have a greater impact.
Here is a picture of my housemates and I enjoying the brownies that we baked. It took longer than expected but it allowed us to chat, laugh, and relax while enjoying the process.
4. Planning ahead to ensure you have sufficient groceries
I usually travel on the bus to get my groceries over the weekend, as it is nice to browse and select my items. However, it can be a little time-consuming when it is ‘crunch time’ due to the additional time spent on commuting. It is helpful to plan and purchase additional groceries with a longer shelf-life to last for the upcoming week. Another helpful way is to purchase your groceries online. There are various stores online, such as Instacart, Weeee, etc that are helpful when other factors are deterring you from going out.
5. Be a little more courageous
That’s what I tell myself when I do not understand the concepts or have questions about the topic being taught in class. It could be my personality or how I am used to academic lessons back home that make it more challenging for me to ask questions. However, I would encourage you to raise your hand and ask, or go to an office hour appointment to clear the doubts that you may have. If you don’t, the person that is at the losing end will eventually be yourself. As they say, knowledge is power, so do not leave the module with an unanswered question.
Despite various deadlines that you need to meet, it is important to stop and pause, and also look at your surroundings as you commute on the shuttle bus or to your apartment. LA has very beautiful sunsets and skies, but you will miss it if you are just focused on thinking about your to-do list.

Sunset on the way to an evening class
⋯

A Day in the Life of an E-OTD Student Vlog ⟩
August 6, 2024, by Shivani
Classes School/Life Balance
Ever wonder what it’s like to be an E-OTD student at USC Chan? Well, I’m here to show you!
Prior to starting grad school, I was a nervous wreck because I didn’t know what was in store for me. However, over time, I was able to realize that I have the ability to shape my grad school experience. Being a part of the USC Chan Trojan Family has been such a rewarding experience thus far, as it has taught me that being a student doesn’t need to consume my entire experience. Grad school is also the time to discover who you are and make memories that will last a lifetime.
I hope my short vlog is able to show you the lighthearted, fun, and exciting aspects of grad school! My journey has transformed from initial uncertainty to a fulfilling and balanced experience, and I’m so excited to share it with you. Thanks for watching and being a part of my grad school journey, and as always, Fight On!
⋯





