Student Blog
Fieldwork
Vivir Con Diabetes ⟩
May 25, 2021, by Global Initiatives Team
Diversity Fieldwork Getting Involved
By Stephanie Gomez-Rubalcava and Liz Rivera
Professional Master’s students
Vivir Con Diabetes (in English: “Living With Diabetes”) is a community service project that we have been hosting as a part of the Albert Schweitzer Fellowship. This fellowship requires students to collaborate with a community site and create a project that caters to the needs of an underserved population. Our project was tailored to service individuals in the local, Spanish-speaking community of Boyle Heights who have been diagnosed with prediabetes or Type II diabetes. We believe that there is an increased need for healthcare providers who can implement culturally-sensitive interventions.
This program was started in 2018 by an occupational therapy student in the Chan Division, David Saldana. It was then continued the following year by Daniel Padilla Vega and Cecilia Garcia. We began as volunteers for the program in 2019 and were awarded the Schweitzer Fellowship in 2020. With USC OT students receiving this fellowship for the third year, it provided us the opportunity to continue expanding this amazing work. Our sessions covered topics related to lifestyle modifications to improve diabetes management such as: stress management, mental health, sleep hygiene, and increasing understanding of what it means to be diagnosed with diabetes. We really wanted to focus on prevention for those diagnosed with prediabetes and on modifying the habits and routines of those diagnosed with diabetes. In previous years, these sessions were hosted in person at our project site, the LAC+USC Wellness Center, but due to the global pandemic, we had to host the sessions virtually.
Although over the last year we faced several challenges in delivering the diabetes management content via Zoom, there were some great benefits to conducting this program virtually. Some of the challenges included making the program accessible for our target population, participant difficulties navigating Zoom, and internet connectivity issues. The silver lining to all of these challenges was that over the weeks, we created a family-like, virtual community and provided participants with space to reflect on their health goals. Many of them mentioned that our Saturday sessions were the only time they dedicated to themselves, and so we decided to incorporate at least 10 minutes of mindfulness/yoga activities to each session. We also provided every participant with at least one free, at-home hemoglobin A1c test to screen for diabetes.
Although a couple of weeks ago we celebrated our final Vivir Con Diabetes session, we are truly grateful for the opportunity to learn with and from our participants. As soon-to-be Latina graduates of occupational therapy, we are excited to continue working with our Latinx community in our future careers and helping them bring about positive and meaningful change in their lives. Lastly, Stephanie Perez, a previous volunteer of Vivir Con Diabetes, has recently been awarded a 2021-2022 Albert Schweitzer Fellowship (see contact information below). We are excited for her to bring innovative ideas to the program, and we encourage current or incoming students to contact her for an opportunity to volunteer with her project during the Fall and Spring semesters. Thank you to our mentor Dr. Jesus Diaz, Daniel, Cecilia, and all of our 2020-2021 student volunteers for making this program possible. Fight on Trojans!
Stephanie Perez, OTS: .(JavaScript must be enabled to view this email address)

A photo from one of our nutrition/healthy eating sessions. We prepared overnight oats with some of the participants via Zoom.
⋯

A Week in the Life: OTD Residency Edition ⟩
April 30, 2021, by Daniel
Classes Fieldwork Life Hacks Videos
As I prepare to go into the last semester of my OTD Residency, I wanted to share with you all what a typical week looks like for me. Completing my residency at the LAC+USC Primary Care Adult West Clinic has been one of the most rewarding experiences I’ve had as a student, and now licensed occupational therapist.
I hope you find this vlog helpful and enjoy it!!!
If you have any questions, feel free to reach out to me at .(JavaScript must be enabled to view this email address) or .(JavaScript must be enabled to view this email address).
⋯

Fighting Feelings of Imposter Syndrome During Fieldwork ⟩
April 9, 2021, by Calvin
Fieldwork What are OS/OT?
Just last week, I completed my first Level II Fieldwork at Prototypes: A Program of HealthRIGHT 360! I was placed with the agency’s Adult Full Service Partnership (FSP) Program and Children’s Program where I was able to provide individualized occupational therapy services to clients across the lifespan who struggle with mental health concerns, needs, and barriers.
This was my first full-time fieldwork placement. I was expected to be there every day from 9:00 AM to 5:30 PM, whereas my previous Level I Fieldwork placements did not require me to come as often. Although I had heard amazing things about Prototypes from previous fieldwork students, I knew that things would be different given the pandemic situation, and also just that everyone’s experience is different. I was feeling anxious about taking on telehealth services, potentially meeting clients in-person, documentation, and more. I wasn’t sure how I would fit in with the team or if I was going to represent OT well enough in the mental health field. The imposter syndrome was real. However, after my first few weeks of fieldwork, those feelings of impostorism gradually began to fade away. I was able to build my confidence to thrive in what turned out to be a beyond-stellar fieldwork experience.
My clinical instructor (CI) was the only occupational therapist at my site, but they truly advocated and raised OT awareness within our client and provider population. I am so fortunate to have had their supervision because they helped further my understanding of what occupational therapy’s role in mental health is. I also appreciated how they always challenged me to ask questions and tested my clinical reasoning and critical thinking skills. At first, I was nervous about making mistakes, but I kept reminding myself that it’s okay and that I should take those as opportunities to learn and grow. Additionally, with the rest of the agency team (inclusive of case managers, clinicians, administrative support and program directors), I felt very well supported and empowered to make an impact as an occupational therapy fieldwork student. It wasn’t long after the beginning when I started to more confidently plan clients’ treatments, document my sessions, present cases to my fellow colleagues, and really highlight the unique capacity of occupational therapy within the mental health community.
It was this sense of community and appreciation for OT that made me feel like I belonged, and uplifted me to bring my skills and knowledge of resources to the table. I was able to creatively collaborate with my caseload of clients to address hygiene management, budgeting their finances, accessing resources, accountability with task completion, social participation, engaging in habit change, and building and maintaining routines so that they can independently participate in their daily lives. I realized that this is the beautiful work of occupational therapy in mental health (and of course there’s so much more to it)! These are meaningful occupations that may be difficult for individuals to participate in because of their mental health needs and barriers. As occupational therapists, we have the power to use occupations as a means and as an ends, as well as to support our clients with health promotion and education, holistic interventions, and our therapeutic use of self.
Overcoming self-doubt and persevering through my own imposter syndrome enabled me to come out of this fieldwork with a wealth of insight, about OT and about myself. I’m grateful for My Mental Health Immersion Experience for providing me with such a solid foundation that prepared me well for this experience. Also, the interprofessional collaboration that I experienced here was extraordinary, and I am incredibly thankful for all the mental health practitioners that I was able to collaborate with. Finally, thank you to my CI, my new West Coast University OT student friends, and especially my ambassador teammate, Bethany Yew, who was placed there along with me — WE DID IT, BETHANY!!!
I am very much looking forward to transitioning into my next, and final, Level II Fieldwork for the Summer 2021 semester, and I can’t wait to continue translating everything I’ve learned through my experiences! Whether if it’s our first or last, or if it’s Level I or Level II, good luck to all of us going into fieldwork. Let’s continue to support one another and make the most out of our experiences!
⋯

Mixed Status Families ⟩
March 29, 2021, by Daniel
Admissions Classes Diversity Fieldwork Life Hacks
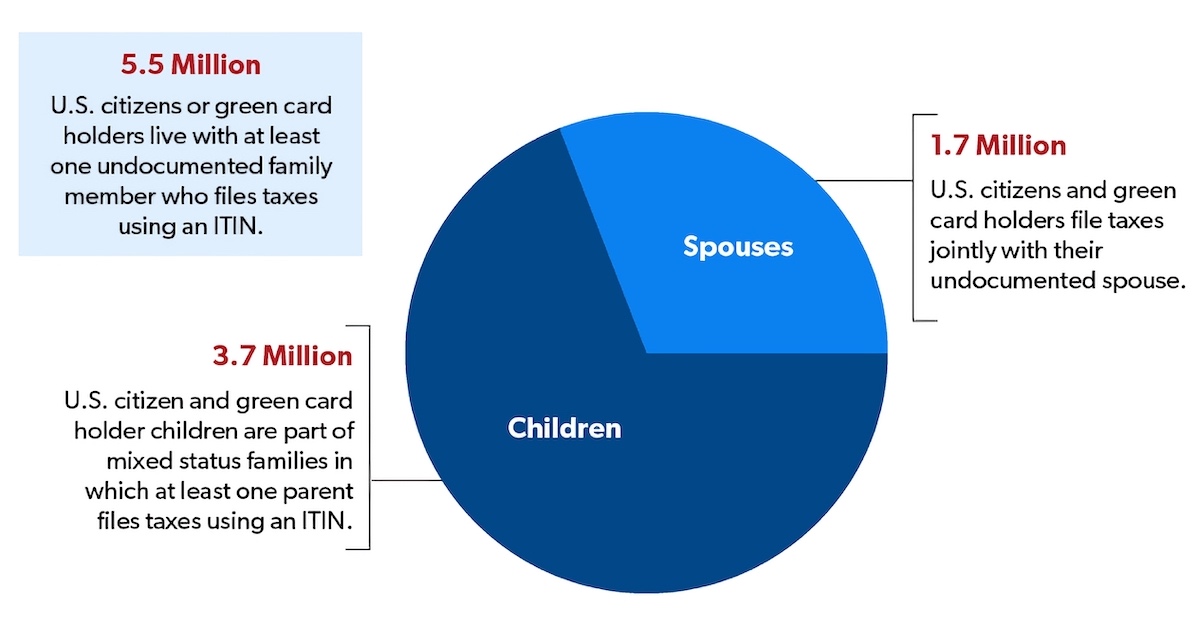
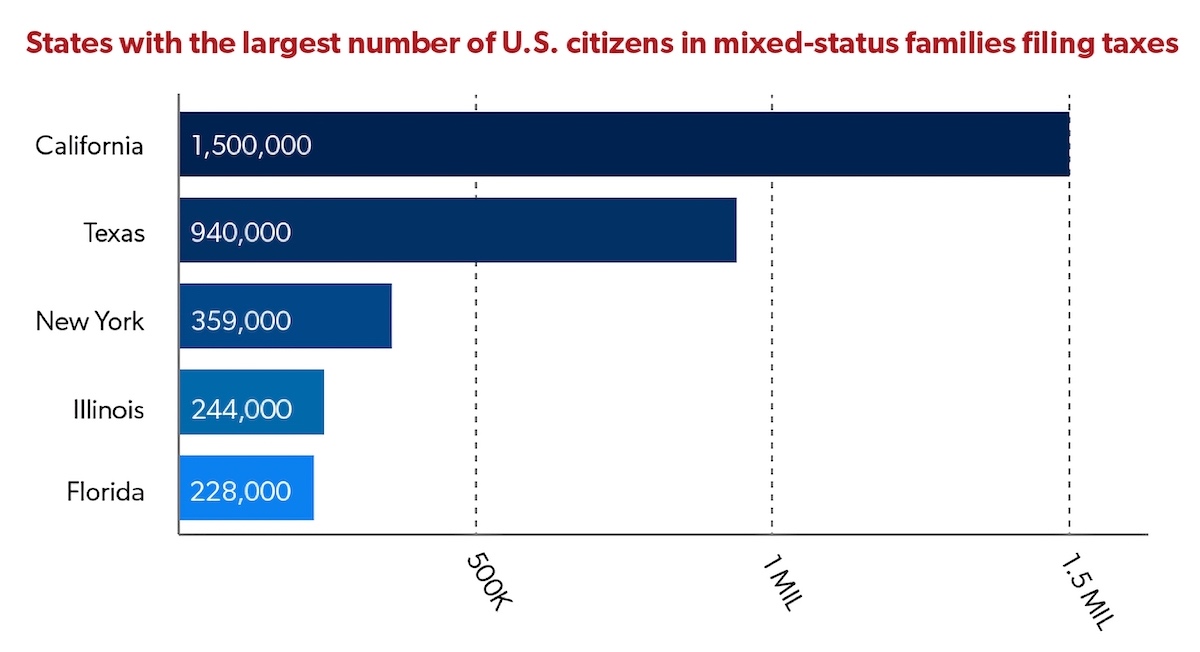
According to the National Immigration Law Center, “a mixed-status family is a family whose members include people with different citizenship or immigration statuses. One example of a mixed-status family is one in which the parents are undocumented, and the children are U.S. born citizens”. The state of California has the largest number of U.S. citizens in mixed status families filing taxes, at 1.5 million people. This is a topic I would like to bring more attention to because many people may come from or know someone from a mixed status family, this includes students at USC and clients seen during fieldwork or residency, and this may not be something that is often brought up in the classroom. Personally, I live in a mixed status family, which includes DACA recipients and people without any documentation, with some extended family having other statuses as well.
Source: Migration Policy Institute, “Mixed-Status Families Ineligible for CARES Act Federal Pandemic Stimulus Checks” (May 2020), migrationpolicy.org/content/mixed-status-families-ineligible-pandemic-stimulus-checks
Source: Migration Policy Institute, “Vulnerable to COVID-19 and in Frontline Jobs, Immigrants Are Mostly Shut Out of U.S. Relief” (April 24, 2020) migrationpolicy.org/article/covid19-immigrants-shut-out-federal-relief
This past year has been really tough financially for my family and me. The multiple stimulus packages that were passed came with a lot of limitations for mixed status families. For example, as a USC student who is undocumented with DACA status, I was unable to apply to the CARES Act financial assistance for college students. After doing some research and waiting for the final relief bills to be amended and passed, I was fortunate to receive the stimulus check because I have a temporary work permit via DACA. However, not all undocumented students are DACA recipients, and many undocumented people did not qualify for anything, even though they pay taxes every year with an Individual Taxpayer Identification Number (ITIN) number. In the last year, I saw many people be excluded from federal assistance simply because of their immigration status, personally at home, with friends, and at residency. My parents and many of my clients in primary care were impacted by the exclusions in the COVID-19 relief bills, including the most recent under the Biden administration.
During this time, many families continue to rely on food banks, are behind on rent, and are surviving on the little help they can get. For example, I helped my parents and some of my clients apply to local and state specific relief programs which provided some financial assistance, but not nearly enough. And for many it’s not an easy process due to technology access, literacy levels, social support, etc. Last fall, I helped my parents write a letter and email it to a rent relief program that provided $500. I was appreciative that non-profit organizations and certain school departments took it upon themselves to be more inclusive and provide some type of financial assistance for students that may have not qualified for the CARES Act. As a current student, I was able to apply for the USC Ostrow Emergency Fund, the USC Graduate Student Government Emergency Assistance, and Immigranted (non-profit organization) for financial assistance to get through the year. Most of that assistance and my stimulus checks went to home expenses that my parents were simply unable to cover.
I believe this is an important discussion we need to have or at least consider in the academic setting and occupational therapy world. As I stated earlier, this impacts students at USC and in the OT programs, as well as clients being seen by occupational therapists/residents and/or fieldwork students. It’s important to consider how students may be navigating their own experience within a mixed-status family or perhaps have family/friends, clients, or colleagues that are experiencing this. As the Chan Division continues to push for more diversity and students from different backgrounds come in, it’s important to consider how prepared we are to support their education and clinical experience within the context discussed above.
No matter your political views, from an occupational therapy lens, we all have a responsibility to promote occupational engagement and occupational justice. This may include supporting clients navigating access to resources. As I found myself doing with my family and clients in primary care, I was that person that supported their own resource seeking as a means for survival during the pandemic. The reality is that not everyone has access to OT services or a family member who can help them seek resources. This is a very complex topic and there are many layers to it, perhaps many terms you may not be familiar with. I am always available for any questions (.(JavaScript must be enabled to view this email address)). I ask you to be open minded and encourage you to have these uncomfortable conversations. It is never too late to start learning and getting involved in the discussion. The COVID-19 pandemic revealed and exacerbated many of the disparities and social inequalities that have been there for many people in the United States, especially the undocumented population. I want to leave you with the questions below to reflect on:
- As a current or future occupational therapist, how are you going to support clients experiencing occupational injustices due to their immigration status?
- How are the needs of students within mixed-status families being met? How can we best support them in reaching their educational and professional goals?
References
Chishti, M., & Bolter, J. (2020, December 11). Vulnerable to COVID-19 and in Frontline Jobs, Immigrants Are Mostly Shut Out of U.S. Relief. Migrationpolicy.Org. https://migrationpolicy.org/article/covid19-immigrants-shut-out-federal-relief
Fact Sheet: Mixed Status Families and COVID-19 Economic Relief. (2020, August 13). National Immigration Forum. https://immigrationforum.org/article/mixed-status-families-and-covid-19-economic-relief
Mixed-Status Families Ineligible for CARES Act Federal Pandemic Stimulus Checks. (2020, December 9). Migrationpolicy.Org. https://migrationpolicy.org/content/mixed-status-families-ineligible-pandemic-stimulus-checks
The Affordable Care Act & Mixed-Status Families. (2017, October 20). National Immigration Law Center. https://nilc.org/issues/health-care/aca_mixedstatusfams
⋯

Level II Fieldwork Part I: Almost Complete! ⟩
March 26, 2021, by Liz
Fieldwork
I am so bummed that level II fieldwork is almost over—one week to go! 12 weeks literally flew by. If you read my previous blog post about my level II fieldwork placement, I’ve been having a blast the past 3 months. I can confidently say that I feel prepared to practice in a hand therapy setting! Here’s a little bit of what I’ve learned these past three months:
How to complete an initial evaluation
This is so important y’all. Not only is it key for knowing why the patient is coming in/what their primary complaint is, but it is the first interaction that you have with them. This is your chance to begin creating that relationship. At first I was a little nervous. I was so grateful for masks because it made it that much easier to hide how nervous I felt! But, I’ve done so many initial evals that now it’s a piece of cake. There’s so many important questions to ask: have you had surgery? Any steroid injections? How does this affect your ability to do things every day? Do you currently own a splint? Take measurements as needed. And yes, these are all super important, but so is the impression you make. This will determine how comfortable the patient will feel with—can they trust you?
How to explain to patients what in the world is going on
A lot of times patients will come in and have no clue what’s going on. This is why knowing your anatomy and familiarizing yourself with diagnoses is critical. You also have to keep in mind that patients will not usually know what in the world extensor carpi radialis brevis is. Explain in a way that the patient will actually understand! Practicing this is super helpful for when patients say “what is tennis elbow, I don’t even play tennis!”
Prioritize occupations!
I’ve seen folks who come in post surgery and also those who are trying to take care of their condition conservatively. In both cases, I’ve had people ask if they need to stop doing things they love. In some cases, the goal is to get them back to doing those things. I had a client who fractured one of his carpal bones and hasn’t been able to surf for months. Attempting to surf right now probably wouldn’t be the best idea. But, what we’ve been working on is getting his range of motion back and slowly working towards weight bearing so he can push off on his surfboard, wax it, put on his wetsuit, etc.
Documentation
We learned a little bit about this in the hands electives and in adult rehab as well. This is super important for noting what you did with the patient, how they responded to treatment/modalities, what happened, why do they need to continue coming to OT. This looks differently at each site, but to date I’ve written so many SOAP notes I already lost count! SOAP notes are used in several OT settings. It stands for: Subjective, Objective, Assessment, and Plan. These provide information about what the patient said/what they’re reporting, what you observed/measured as a skilled clinician, why they still need to continue seeing you, how are they progressing?, and what the plan is for the next session. You’ll learned more about this when you practice writing SOAP notes in class. 😊
How to actually treat people
Anyone can Google what a trigger finger is. But, what do you actually do when a client comes in with one? This is when I was super grateful for my fieldwork educator. There’s a reason why practicing in a hands setting is considered advanced practice. There’s so much! There’s a lot to know, and everyone’s conditions may present similarly but also be very different. I’ve had the chance to independently treat so many diagnoses including: trigger fingers, wrist fractures, Dupytren’s contractures, carpal tunnel, rheumatoid arthritis, osteoarthritis, cubital tunnel, tennis elbow and even a couple folks who have had amputations—to name a few. I am very happy to say that I’ve felt completely comfortable treating these conditions.
Splints 101
Making splints is tough y’all! It is literally art. For one, there’s different materials to choose from. Some cool faster than others, some are more comfortable for night wear, others are more restrictive. I had the chance to make a couple short opponens splints and a few trigger finger splints as well. My fieldwork educator has so much experience and I’ve seen him create some amazing splints for different people. Making splints is great, but with that comes some client education. Can they bathe with it? Should they sleep with it? Skin checks! Tip #1: Don’t leave it in your car—it might lose its shape with the heat!
Being confident in myself
It’s okay to not know everything. It’s literally been only three months! At first it was rough to come to terms that I wasn’t an expert. But, now that I’ve really got the hang of everything I am so sad that this placement is coming to an end! I’ve learned that it’s okay not to know everything and asking questions is fine. My fieldwork educator once told me, “You might not know it all, but you definitely know more than the patient so believe in yourself”.
So, this is all just a fraction of what I’ve learned so far. After nearly a year of learning from behind a screen, I am so grateful for this experience. It exceeded my expectations of what level II fieldwork would be like. If you have any questions about my placement or want to know more about my experience please feel free to shoot me an email!
⋯