Student Blog
Fieldwork

When a Planner’s Plan Doesn’t go to Plan ⟩
July 21, 2020, by Savi
Fieldwork What are OS/OT?
You never know where you are going to end up. This was a comment I heard from a lot of USC faculty and staff during my first summer in the Master’s program. I would chuckle and dismiss these comments because I have always known what setting I wanted to work in as an occupational therapist (OT). When I have a plan I rarely sway from it. After deciding to pursue a career as an OT in acute care during my junior year of high school, I did everything I could to fulfill this dream of mine.
Upon entering into my first immersion, mental health, I had already convinced myself that this was not the field I was going to work in. As I attended more classes, participated in group discussions, and immersed myself in an eye-opening fieldwork placement, I soon came to realize that my plan to pursue a career in acute care may not be my goal after all. In this fieldwork setting I listened to my clients’ stories and worked with them to overcome the mental health barriers they faced to become better mothers. This experience made me realize that my love for working with clients to improve both mental and physical health in order to engage in meaningful occupations can be applied in a variety of settings. For the first time in a while, I was confused about where I was going to end up, and that made me feel uneasy.
It was not until I was introduced to my faculty mentor, Kimberly Perring Lenington, that I came to terms with the fact that my confusion was a good thing and not something to be afraid of. I instantly admired Dr. Lenington for achieving my original goal of working in the acute care setting directly after graduating from USC. I remember asking Dr. Lenington if this was her goal all along and recall her explaining that this was not her plan. She fell into this setting and loves it. I was shocked. I didn’t have to plan my entire career from high school in order to be successful in my field of choice?
While learning more about Dr. Lenington I discovered a niche specialty I was never aware of. Dr. Lenington also treats individuals with various pelvic health diagnoses including incontinence, pelvic pain, and sexual dysfunction. After diving deeper into this pelvic health specialty and learning more about OT’s role in sexual health in my OT 534 Health Promotion and Wellness course, I became fascinated by the opportunity to work with women to help them holistically. In this setting, I could tackle the mental and physical barriers to achieving pelvic health in order to help women participate in meaningful occupations. Let’s just say I was immediately hooked!
Although I am still passionate about the possibility of working in an acute care setting, I have come to the understanding that I must allow myself to keep an open mind. Without doing so I would have never discovered the pelvic health specialty that I am now extremely excited about. It is ok to be confused about where you want to be once you graduate. This confusion is truly a gift. Allowing yourself to keep an open mind, in turn, widens the realm of possibilities. So to those who are planners like me, know that it is all right to redo your plan. Keep your options open . . . you never know what opportunities could be coming your way!
⋯

Communication is Key!!! Especially in Telehealth! ⟩
July 15, 2020, by Daniel
Fieldwork
Good communication is an important skill that all occupational therapists need to develop and continue to improve as they continue to practice. As a student completing my final level-2 fieldwork at LAC+USC Adult West Primary Care Clinic, I’ve had the opportunity to practice my communication skills every day. Especially now that most settings are providing telehealth, communication is vital to making things work! The most difficult part about working remotely and communicating is that you may have never actually met the person you are talking to. My time at fieldwork this summer has consisted of communicating with patients over the phone, and communicating with the primary care team via phone, email, video camera, and messages.
Communicating with patients:
One of the hardest things I’ve had to do as an occupational therapy (OT) student is facilitate a one on one, 1-hour appointment over the phone with someone I have never met before. Whether it’s an initial evaluation, progress phone visit, or discharge, asking someone to answer all your questions and trust you over the phone is a lot to ask! Furthermore, if patients have had previous negative experiences in the healthcare system, they may be reluctant to opening up to you. Neither of you are able to see each other’s body language or pick up on cues that people rely on when having a conversation. The way you frame questions, your tone of voice, and your ability to listen will be key to communicate effectively! When I think back to all of the courses I have taken at USC, I have to say that OT 578 Therapeutic Communication: Facilitating Change in Clients (Motivational Interviewing) with Dr. Diaz is one of the most valuable courses I have taken in my entire college career. This class taught me the importance of simply listening to someone and showing them that you care by using reflections, affirmations, summaries, etc. in order to build that trusting relationship with your patient. This may be the first time a healthcare provider is actually taking the time to listen to them and agreeing with a lot of the frustrations they may be expressing. Additionally, the structure in the primary care clinic allows OT to spend up to an hour talking about making lifestyle changes with a patient. This client-centered approach of focusing on the patient’s needs and wants is the unique value of OT. The reality is that motivational interviewing may not work for every single one of your patients, but it is an evidence-based approach that I have personally found valuable during my time in primary care.
Communicating with your team:
Again, communication, communication! At the clinic our interdisciplinary team consists of primary care providers (medical doctors, physician assistants, nurse practitioners), clinical pharmacists, certified medical assistants (CMAs) community health workers (CHWs), care managers, nurses, medical case workers (MCWs), 1 occupational therapist, and 1 occupational therapy student (me). Working within an interdisciplinary team can be challenging at first. My first couple of weeks in fieldwork I spent learning how to use the communication systems used by LAC+USC County, which was frustrating at times with IT or technology issues. In the beginning, every electronic medical record (EMR) message or email I would send to a patient’s primary care provider (PCP) would make me nervous because I would be talking to doctors or specialists that have been practicing for a long time. Furthermore, I am communicating sensitive information that can affect the patient if it’s not communicated properly. Once I became more comfortable and got over my fear of “messing up”, I was able to better understand the value of OT and how to effectively communicate patient concerns with the interdisciplinary team. For example, while working with patients diagnosed with uncontrolled diabetes and/or uncontrolled hypertension, we may communicate patient concerns such as hypoglycemia episodes (really low blood sugar levels), not taking medications, reported pain that is limiting their function, and needed support for food and/or housing insecurity as well as financial support. This communication allows us to catch things that the patient may not have reported during their appointments with other providers and help the team provide the best possible care to the patient.
You will make mistakes and that is totally okay! As a student, this is the time to learn from your mistakes and develop those skills that will help you become an amazing OT in the future! As students we are often too hard on ourselves and are afraid to mess up, but remember to take a step back and remind yourself that you are still learning! As long as you are following safety precautions and working with your team to improve your skills, you will become more comfortable communicating with your patients and your team. As many of you begin to go back to fieldwork in the Fall and then begin level-2 fieldwork next year, you will have the support you need from the fieldwork educators, your clinical instructor (CI), and the rest of the team (wherever your setting is) you are working with! I have been fortunate to have such a supportive team at the Adult West primary care clinic with helping me transition into working remotely and providing feedback to develop the necessary skills to work in this setting. I hope this provides some insight into the importance of communication in the world of telehealth! This is a skill that you will be able to develop during the Master’s program and further enhance if you choose to pursue the OTD as you will have additional mentorship from faculty! I hope that no matter what route you choose, that you feel competent when applying to jobs in the future that require great communication skills and telehealth experience.
⋯

Meaningful Occupations and Routine Changes During Quarantine ⟩
July 1, 2020, by Daniel
Fieldwork Life Hacks
During the COVID-19 pandemic many of us have lost our normal routines and had to either adapt or stop engaging in certain daily occupations. Occupations are activities that we need to do, want to do, or are expected to do in our everyday lives. Everyone has a different definition for what a meaningful occupation is, for example, going to school, working, taking walks, interacting in the community, etc. Social distancing has changed the way we work, socialize, and how we take care of ourselves. Right now, more than ever, occupational therapy plays a crucial role in guiding patients through the process of creating and/or adjusting habits and routines that are personally meaningful and health promoting. Occupational therapy has the ability to address the physical, mental, and spiritual wellbeing of individuals.
During my remote fieldwork at the LAC+USC Adult West clinic, I have had many conversations regarding increased levels of fear, anxiety, anger, and depression. These are completely normal feelings to have during a time of so much uncertainty. People are worried about their health, financial responsibilities, food insecurity, their loved ones, social injustice, etc. Furthermore, the inability to engage in their usual daily occupations has taken a toll on many of the patients at the clinic. Yet, it is important that we do not let these feelings control our lives, and instead, find healthy ways to cope with these feelings and find ways to begin to engage in meaningful occupations. For example, many people are worried about not being able to work which leads to stress and anxiety about how they will provide for their families the longer this continues. To many this is an extreme change in their lives and are not able to engage in what they have considered a meaningful occupation (working) for the last 10-20 years. Often, our phone visits will focus on exploring coping strategies to manage stress or anxiety, and connecting them to resources that may support them with basic necessities. Without the ability to take care of their basic needs, patients have difficulty focusing on managing their health. Furthermore, we support patients by finding ways to increase activity level and engage in safe/appropriate socialization.
Below are some resources that you can use with your future patients and for yourself:
Patient Resources:
- My Therapist Aid: A tool for mental health professionals that includes worksheets, audio, videos, guides, interactive activities, and products. Resources can be searched by topic to tailor activities to client’s needs (i.e. stress, anger, anxiety, depression, grief, self-esteem, relaxation, substance abuse, etc.).
- Mindful USC: free app with guided meditations, as well as information about mindfulness classes, retreats and events in the community.
- UCLA Guided Meditations: different types of free meditations in English and Spanish, that can be played as audio or read using a transcript. The meditations can also be accessed via the “UCLA Mindful” app for free.
- YouTube meditations: YouTube is a great resource for many of our patients because it is free and it has so many options! Patients can explore different types of meditations such as guided meditations, sleep meditations, meditations with music, etc.
- Deep Breathing: a relaxation technique that focuses on taking slow deep breaths to provide relief from stress and anxiety. This reminds you to breathe, bring that heart rate down, and relax your muscles.
- 211LA: A hub for community members and community organizations looking for all types of health, human, and social services in Los Angeles County.
Personal Coping Strategies:
- Music/Lo-Fi Music: Music has always been a coping strategy for stress and anxiety for many years. More recently, I really enjoyed simply playing lo-fi music, which is a type of music that is mostly beats.
- Exercise: Strengthening exercises and running have been one of my biggest coping strategies during moments of stress. Since gyms began to close, I had to re-invent the way that I exercised at home. I started to do more bodyweight exercises and lots of stretching!
- Reading: I know this probably sound exhausting because we usually already have so much to read for school or work! However, I have found it therapeutic to spend at least 20 minutes per day reading books I have genuine interest for and does not feel like more work. A strategy I have been implementing is setting a timer for 20 minutes to read every day.
As I reflect back on the first 7 weeks of fieldwork, I have learned a lot from hearing patients’ personal experiences under these life-changing circumstances. This has been a challenge as I try to support them through a computer monitor and phone. However, this experience has also improved my problem solving, communication, and collaboration skills as the clinic team finds ways to better support patients. This experience has served as a reminder that occupational therapy provides the adequate training to help with challenges that occur when a person is confined to home and is unable to engage in their meaningful occupations.
⋯

A Busy Day in Primary Care Fieldwork — from Home! ⟩
June 11, 2020, by Daniel
Fieldwork Life Hacks
This summer I am doing my level 2 fieldwork with my OTD residency site under the Lifestyle Redesign for Chronic Conditions Lab (LRCC) in primary care at the LAC+USC Adult West Clinic. This OTD residency is designed to expand occupational therapy (OT) services in primary care, focused on addressing chronic condition management among patients with diabetes and/or hypertension, using a Lifestyle Redesign® approach. This summer I am being trained by the current OTD Resident in preparation to take over the full caseload this Fall.
Currently, the primary care clinic does not have a video platform and we are not allowed to use Zoom to interact with patients, thus all of the appointments are three-way phone visits using Doximity (HIPAA compliant) with supervision from my clinical instructor (CI) through the phone and Zoom. I am able to lead appointments in English and Spanish, which is valuable for our predominantly Spanish speaking community at the clinic. The phone visits can be beneficial for some patients as they don’t have to travel far to get to their appointments and can talk to their providers from the comfort of their home. However, there are also barriers for our patients such as not having a quiet space at home or disconnected phone lines due to being unable to pay their phone bill as a result of the pandemic. We do our best to contact all our patients and provide as much support as possible to help them navigate these barriers and be able to manage their health.
Each day can look very different when doing telehealth in primary care, and below I wanted to share an example of a typical busy Wednesday! On this particular day, I started my day with an OTFP in-service learning about mental health when utilizing Lifestyle Redesign® approaches. Next, my CI and I started calling patients since we had done chart reviews the day before. During our phone visits, we discussed topics such as healthy eating, physical activity, stress management, medication adherence, habits and routines, resources, etc., to support their diabetes and/or hypertension diagnosis and overall health management. In the middle of the day we had consecutive meetings to discuss patient progress and how to better support them (care management); fieldwork/residency updates, logistics, and an opportunity to ask for guidance with clinical approaches (fieldwork supervision); and daily clinic updates and projects (daily brief). And perhaps you are wondering . . . when do you eat? Well, there are days when we don’t get an official lunch break, so we do our best to get food in between meetings! Thereafter, we began calling patients again for the rest of the day and documented in between appointments and during our assigned admin/documentation time at the end of the day.
Typical Wednesday
- 8-9AM – Occupational Therapy Faculty Practice (OTFP) In-Service
- 9-11AM — Patient Phone Visits
- 11AM-12PM — Care Management Meeting
- 12-1PM — Fieldwork Supervision Meeting
- 1:05-1:30PM — Clinic Daily Brief
- 1:30-4PM — Patient Phone Visits
- 4-5PM — Admin Time/Documentation
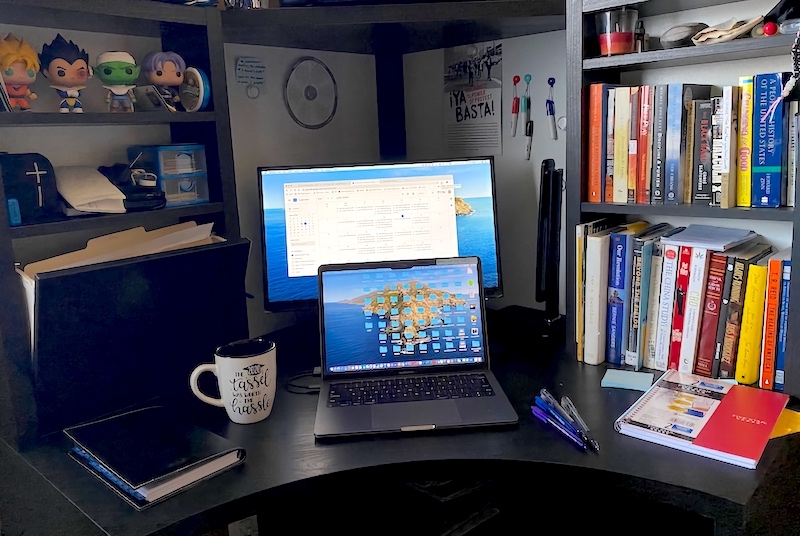
My workspace at home (please don’t judge my ergonomics/set-up, I’m still working on it).
Tips for working from home
- Take stretch breaks: This is one of the most important things you can do for your body. Taking stretch breaks is important to prevent pain, aches, and cramps later on! You can even do stretches while sitting down.
- Snacks & water: Don’t forget to stay hydrated and have snacks in reach to have energy throughout the day!
- Ergonomics: Posture, posture, posture! Please take care of your bodies and follow proper posture and chair tips when working from home. This can easily be overlooked and if you don’t have fancy equipment, there are ways you can get creative! Your body will thank you later.
- Prepare meals: This can save you time on days when you may have a short lunch break or none at all!
I hope this paints a picture of what a busy day of telehealth primary care may look like! My intention is to be transparent with you all and share the good, the bad, and the busy days. I am often exhausted at the end of the day, but I am excited to continue to learn and the patients make it all worth it!
⋯

My First Level 2 Fieldwork (#TBT?) ⟩
November 7, 2019, by Kaho
Fieldwork
I know it’s November and summer feels like ages ago, but with wish-lists for the Summer 2020 level 2 fieldwork about to open up to 1st and 2nd year students, I wanted to reflect and share with you about my fieldwork experience from last summer.
For 12 weeks, I was in an inpatient acute care setting in a hospital in San Diego. As you’d imagine, it was very fast paced, challenging, exciting, etc. and I. Loved. It. Every day looked different and I was constantly learning new things. My clinical instructor (CI) has been an OT for tens of years and working at that specific hospital for over 5 years, but she mentioned that she still learns something new every day. Because the hospital didn’t have a large OT team, the OTs didn’t have an assigned area or floor. The patients in the entire hospital were distributed among the OTs randomly and equally, so I got to see everything from a person with cancer to a patient in neurology to a person with a new hip or a new knee. I was all over the floors, including the Intensive Care Unit (ICU). It was definitely overwhelming at first with so many things to keep in mind and be aware of, and I was nervous to touch anything because it is a setting where careless mistakes could be unforgiving. Also, my level 1 fieldwork was in hand therapy, so this was my first time performing transfers on real patients. However, my CI was amazing at gradually increasing my responsibility and easing me into the bustling hospital halls. She talked me through every treatment session and constantly provided me feedback on my performance. Despite my doubts, I was independently evaluating, treating, and documenting patients by the end of the summer.
My days started at 7:00am and ended at 3:30pm. The first hour of my day consisted of looking up patients’ medical history, condition, precautions, and anything else that was relevant. I was usually up on the floors by 8:00am. I saw about 6-9 patients each day with my CI, depending on how many of them were evaluations since those take longer than regular treatment sessions. In the inpatient acute care setting, your schedule revolves around the patients’ schedules, so documentation occurred during gaps when none of my patients were available or at the end of the day.
One of my favorite things about working in the hospital was that there were many opportunities for collaboration across health care professions. I got to talk to and sometimes treat with physical therapists (PTs), speech language pathologists (SLPs), nurses, and even medical doctors (MDs). We would all bounce ideas off of each other to come up with a holistic treatment plan for each unique patient. With collaboration came opportunities for advocacy, as well. I can’t tell you how many times other health professionals and patients referred to me as PT during my fieldwork experience. Patients would say to me, “What, I just had PT. Why are you back?” or “Why are you taking me to the bathroom? I thought you were going to take me walking down the hallways.” Notes from the nurses or MDs would state things like, “Patient walked to bathroom with PT today.” It was frustrating, but it was a great opportunity for me to practice promoting OT and sharing my elevator speech about what OT is and why we’re great. 😊
Another exciting aspect of having fieldwork in acute care was watching surgeries. I got to watch four surgeries over the summer: a total hip replacement, a total knee replacement, spine surgery, and a deep brain stimulation. It was an incredible learning experience and it deepened my understanding of what surgical patients go through and how much pain they may be experiencing afterwards. It made seeing the patients’ joys of taking their first shower after surgery or being able to get to the edge of their bed and sit without support that much more meaningful.
Whether this is your first level 2 fieldwork or your second, consider the inpatient acute care setting at any hospital if all or any of this sounds intriguing to you. I had a very positive experience and I highly recommend it!
⋯





