Student Blog
Classes

Electing Your Electives ⟩
November 19, 2019, by Catherine
Classes
I’ve been getting a lot of questions about electives. While I highly recommend you take elective based on your interests and intended area of practice, it might be helpful to talk about the electives I took and my experience from them.
OT-572 Ergonomics. I always had a keen interest for ergo, not only to enhance my knowledge to make recommendations for my clients, but I found it incredibly useful in my personal life as well. This is a real hands on course, where you get to practice your ergonomic evaluation skills and also get creative. With the knowledge and skills gained from the class, I re-did all the home workstations of my family members and got rave reviews on how their pain and fatigue had improved. So it was totally worth it!
OT-578 Therapeutic Communication for the Healthcare Practitioner. I took this course because at the time, I was not confident about my interpersonal skills in practice. I was intending on doing my second level II fieldwork in either mental health or adult rehab, and I was looking for a way to get more comfortable putting my best therapeutic use of self forward. This course primarily focused on principles and the practice of motivational interviewing. While you do also get to practice other forms of therapeutic communication such as mindfulness and cognitive behavioral therapy, MI is really the meat of the course. At first, I felt a little awkward, because again, you get A LOT of practice using these skills on each other, but by the end of the course, I felt a lot more comfortable speaking to clients during my fieldwork!
OT-583 Lifestyle Redesign. I chose to take this course because not only was I interested in learning more about our practice methods in health and wellness, but it is one of the signature course offered here at Chan. You get a lot of insight in working with a wide variety of clients who are not only working towards wellness goals such as stress management, weight loss and chronic pain, but I loved learning about emerging evidence based practice in green wellness and corporate wellness. I used the skills I learned in this elective to complete my level II fieldwork project, investigating workplace wellness at my site.
What’s really great about the curriculum at Chan (this goes for both the OTD and MA programs) is that we have A TON of choices. You don’t have to be limited to only the courses offered by the Division but other departments as well, and there is also to option of an independent study. So if you are waitlisted for an elective that you want to take or don’t have an elective that totally speaks to your learning goals, it may be a good idea to peruse the course catalogue and also make an appointment with your mentor for more guidance.
⋯

Craving Crafts? ⟩
September 25, 2019, by Kevin
Classes Life Hacks
It’s no secret that OT 406 Foundations: Creativity, Craft and Activity is one of the most fun courses during your first summer session for the Entry-Level Professional Master’s. Unfortunately, the summer is over and the crafts have been put away, but that doesn’t mean you have to stop crafting and letting that creativity flow! Here is one my favorite crafts to help satisfy your crafting craving.

Memory Coasters
Have some pictures laying around that you would like to display creatively in your home? These memory coasters are the perfect way to show-off all those “instagramable” locations and start a conversation at dinner.
Materials needed
- Scissors
- Self-sealing lamination sheets or laminator
- Pictures
- One-Piece Mason Jar Lids, Wide Mouth
- EastCast Clear Epoxy
- Plastic Cups
- Stirring Sticks
- Gloves
- Wax Paper
- Double-sided Tape
- Marker
Directions
- Trace a circle around the portion of your photo you want to place in your coaster using the bottom of the Mason jar lid.
- Cut out the circle you just traced, then laminate your photo using either a lamination machine or self-sealing lamination sheets. Laminating the photo is an important step, as sunlight and the clear resin will pull the color out of the photo if not protected.
- Cut the laminated photo out a second time and secure the photo in the bottom of the Mason jar lid using adhesive or double-sided tape.
- Place Mason jar lids on a double layer of wax paper to protect the surface you are working on.
- Mix the clear epoxy resin using the directions provided with your resin and be sure to wear gloves and an apron to protect your skin and clothes. Pour epoxy resin into the Mason jar lids until the lid is about halfway full.
- Allow the epoxy resin to dry indoors where the coasters will not be disturbed for about 72 hours. Finally, pour yourself a drink and enjoy your beautiful memory coaster.
⋯

Course Catalogue Queen ⟩
September 9, 2019, by Noelle
Classes Life Hacks
During my first advisement meeting of college, I was told that the credits I brought in from high school allowed me to double major, double minor, or potentially do both! As an eager freshman, I took that statement as suggestion and immediately threw myself into the USC catalogue, frantically scribbling lists of interesting classes, minor and major unit requirements etc. Two hours, about 80 tabs, and 3 existential crises later, I paused to survey my lists hoping to see a clear path. What I ended up with was the opposite — one or two classes in a whole bunch of schools/studies. It was then when I asked myself, “Why am I doing this? Do I actually want to minor in something, or do I just want to be able to say I did?” It was an important question and I’m glad I checked myself. I had spent the previous four years doing everything I thought I had to do to get into a good school, including a lot of things I didn’t really want to do. I don’t regret that at all because it got me where I am, but as I contemplated what I wanted out of the next four years, I realized that it would be dangerous to continue to do things just “for the resume”. After all, I was at USC and there are endless things to engage in that are both personally and professionally fulfilling. I recognized that college was a rare time in life to take risks and explore new subjects and it would be a waste of time and opportunity to be bound to what other people see as prestigious and how they measure success. So, I took my lists of classes and ran. I was introduced to new occupations like ballroom dance, drums, and ceramics. I challenged myself and took financial and managerial accounting and web design. And I looked for opportunities to expand my perspective on health in eastern medicine, bionics, gerontology, and health promotion classes.
I was spoiled in undergrad and I know it. And I am grateful that my hodgepodge of interests is an asset to my future practice as an OT. I’ve noticed a similar trend in my classmates in the division. I am surrounded by people who studied philosophy, marketing, biology, who teach yoga classes, build puzzles, served in the military, and had multiple careers before coming to OT school. We are an interesting bunch her at Chan, and we all share the value of meaningful engagement for the clients we serve and ourselves.
Check out Visions and Voices, Sidney Harman Academy for Polymathic Study, and the Ahmanson Lab for some interdisciplinary activities available to undergrad/grad students and alumni.
This week’s song pick: “Back Pocket” by Vulfpeck
⋯

Electives: OT Generalist to Specialist ⟩
April 17, 2019, by Jessica P.
Classes
In the spring semester of the second-year in the Master’s program, we get the opportunity to take elective courses. Like all OT programs, USC Chan prepares us to be OT generalists when we graduate, but we also get to take 12-14 units of elective coursework. These courses allow us to begin to focus in an area of interest, taking you from an OT generalist to specialist. Our division offers over 20 electives and also gives us the opportunity to take classes outside of the Chan division. For example, if you are interested in opening your own private practice you could take courses in the USC Marshall School of Business or if you are interested in health policy you could take courses in the USC Sol Price School of Public Policy.
I wanted to share a little more in-depth about the electives I chose to take this semester to give you a glimpse at all of the hands-on opportunities I’ve had throughout this semester.
OT 561: Occupational Therapy in Acute Care
In this class we have a lecture portion where we learn about the blend between a top-down occupation-based approach and bottom-up systems-based approach within the context of acute care. In addition to the class, we also get to complete a clinical experience portion at Keck Hospital of USC. At Keck, we get hands-on experience working with occupational therapists in a variety of settings. During my clinical experience, I was fortunate enough to see OTs working in various ICUs, neurology, cardiology, and orthopedics.
OT 573: Hand Rehabilitation
Throughout this course we learned how to blend the art and science of hand therapy in order to first be occupational therapists and then hand therapists. It was very hands-on, using case studies, splinting scenarios, and even a functional anatomy super bowl. Our professor taught us about addressing topics such as wound healing, scar management, physical agent modalities, splinting, peripheral nerve injuries, and arthritis — and most importantly, addressing these topics with an occupation-based approach. For my classmates who are interested in pursuing advanced practice in hands, the hours from this class counts towards their education hours!

One of my classmates, Sarah, practicing applying a plaster digital cast on my finger
OT 574: Enhancing Motor Control for Occupation
This course emphasizes using motor control techniques in order to increase engagement in occupations. For the first four weeks of the semester, we focused on learning basic mobilizations and facilitations on each other utilizing handling skills based on the Neurodevelopment Treatment Approach. After this, we had weekly two-hour treatment sessions with our patient models. These patient models are real people who have all experienced a stroke. Each week, we would develop and implement a treatment plan with our patients as well as give them homework to work on.
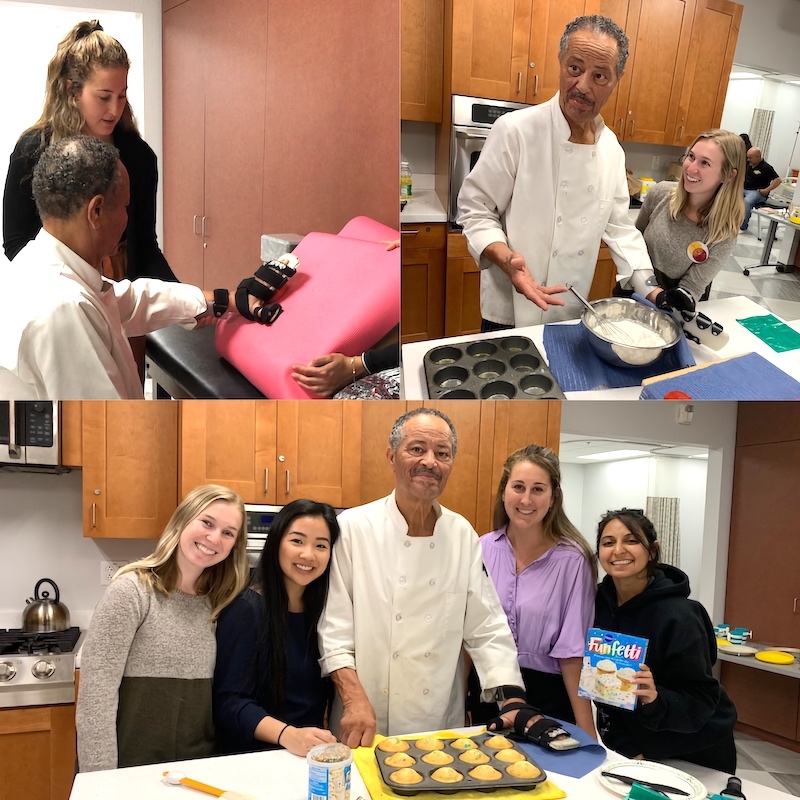
For our last session with Louis, he taught our group to make cupcakes because one of his goals is to be a chef instructor
My group’s patient, Louis, was one of the best teachers I have had in OT school. He allowed us to try out different treatment ideas and was always so motivated to work with us. I learned how to grade treatment sessions to the “just-right challenge” and always have back-up plans. Most importantly, Louis taught me about resilience and the difference that a positive attitude can make on the recovery process.
OT 575: Dysphagia Across the Lifespan
In dysphagia we learned about the anatomy and physiology of the structures involved in swallowing and how this impacts the occupation of eating. We also learned assessment and treatment strategies for patients of all ages in different settings. Through lectures, case studies, and hands-on techniques we learned about how occupational therapists can have a distinct role in approaching dysphagia management. One of my favorite lectures was on performing oral exams and we even got to test our classmates’ gag reflexes! Luckily, since I am interested in pursuing my advanced practice in dysphagia, this course counts towards 24 out of the 45 hours needed for specialization in California.
Throughout all of my classes in the program at USC there has been a strong emphasis on occupation-based approaches. After all occupation is in our job title! The electives I chose to take took it even further with demonstrating how to stay occupation-based in settings or with populations where a bottom-up, biomechanical model may be more typical. I feel so grateful to have had the opportunity to customize my coursework with electives this semester to prepare myself for the areas of practice and specialization I am interested in pursuing.
⋯

And So It Begins . . . One Last Time ⟩
February 4, 2019, by Melissa
Classes
Hey guys! This semester is now in full swing after a wonderful and restful break. For those of you that don’t know, our final semester in the program consists of a variety of electives that allow us to specialize/customize our academic experience! I talk about what that entails in one of my previous posts, so check it out if you’re interested in knowing more!
In this post, I want to talk a bit more in depth about the courses that I am taking, as I find it fascinating that we get this opportunity to customize our learning experience. Although I’ve found our curriculum thus far to be incredibly useful and important for our foundational knowledge of the profession, being able to take courses that I have chosen based on my own personal preferences is amazing! Although I am interested in both pediatrics and adult physical rehabilitation, I chose to focus more on my interests in physical rehab. Thus, I’m taking courses in Primary Care, Acute Care, Neurorehabilitation, and Dysphagia, in addition to our Leadership Capstone, and Occupational Science course. It is definitely a full course load, but I’m enjoying it tremendously.
My Primary Care and Acute Care courses have an additional clinical component in which we get to shadow an occupational therapist in those respective settings. For the Acute class, we get to go across the street to Keck Hospital, where we get to see some incredibly complex cases. The medical complexity surrounding some of the cases we see really adds an additional layer to the problem solving we have to do in our career as OTs. Learning about all of the medical conditions we might encounter in class, and then immediately seeing some of those conditions during our clinical experiences is pretty surreal, but it truly helps to solidify the information that we are learning.

Occupational therapy in primary care is an emerging area for our profession, but it makes complete sense to have OTs in that setting! We learn all about the complexities associated with primary care — particularly surrounding the constantly changing policy and reimbursement challenges — and how that impacts our ability to be included as part of a patient’s care in that setting. For our clinical experiences, we have the option to shadow an OT providing direct care in a primary care setting, or to see what consultative OT looks like as well! Again, being able to apply what we’re learning in class to a real-life situation is amazing, and so helpful for my learning.
Although the Neurorehabilitation and Dysphagia courses don’t have a clinical component, there is still a lot of hands-on learning involved. In Neurorehab, we get to practice different assessments on each other, which is useful because a sense of mastery is necessary to execute these assessments well. In Dysphagia, we learn all about the anatomy associated with swallowing, and also practice swallowing assessments on each other to aid in our knowledge. Another cool thing about the Dysphagia course is that the hours in the course count towards our certification in that area! There is a certain amount of hours that have to be completed as part of that certification, therefore it’s great that we get a head start.
In addition to all of the exciting things going on related to my clinical experiences and electives, I get to look forward to completing my externship in March, welcoming the incoming class in April, and of course graduation in May! I had heard from other students that the Spring semester is a whirlwind that goes by very quickly, and now I definitely know what they mean! If you have any questions about the elective process, any of the specific course, or anything about the program in general, feel free to reach out!
⋯





